I.
Suppose you have sniffles, fatigue, muscle aches, and headache. You go to the doctor, who diagnoses you with influenza and gives you some Tamiflu.
There’s some complicated statistics going on here. Your doctor has noticed some observable variables (sniffles, fatigue, etc) – and inferred the presence of an invisible latent variable (influenza). Then, instead of treating the symptoms with eg aspirin for the headache, she treats the latent variable itself, expecting its effects to disappear along with it.
Psychiatry tries to use the same model. You get some symptoms – depressed mood, insomnia, fatigue, feelings of worthlessness, suicidality. You go to the psychiatrist, who diagnoses you with depression and gives you an antidepressant.
The psychiatrist is implicitly assuming that the causal structure of her field matches the causal structure of better-understood diseases like influenza. Generations of psychiatrists have noticed that different symptoms all tend to show up together and follow a similar pattern, suggesting some kind of deep connection between them. So psychiatrists follow the influenza model and attribute this collection of linked symptoms to a latent variable called “depression”.
This gets complicated really fast. Psychiatric disorders are diagnosed through clusters of symptoms, but we don’t expect every person to have every symptom in the cluster. For example, we diagnose depression when a patient has five out of nine symptoms on a list including fatigue, guilt, sleep disturbance, suicidality, et cetera. Each of these symptoms is often but not always present in a patient who has most of the others – for example, 75% of depressed patients have sleep disturbances, but 25% don’t.
But all psychiatric disorders are hopelessly comorbid with each other. If someone meets criteria for one DSM disorder, there’s a 50% chance they’ll have another one too. 60% of people with major depression also have an anxiety disorder. This is awkward when compared to eg the 75% sleep disturbance rate. Why are we calling sleep disturbance a “symptom” of depression, but anxiety a “comorbid condition” with depression? If we’re trying to cluster symptoms together to identify conditions, how come “sleep” is grouped with a bunch of other symptoms in the depression cluster, but “anxiety” gets to be a cluster of its own? Are there really two conditions called “depression” and “anxiety”, or just one big condition that has various symptoms including low mood, sleep disturbance, and anxiety, and some people get some of the symptoms and other people get others? I’m told that the people who write the DSM have long conversations about this using rigorous methods, but to the rest of us it seems kind of arbitrary.
The problem isn’t that nothing ever clusters together – depression, for example, is a very natural category. But so are various subtypes of depression. And so are various supertypes of depression, like depression + anxiety, or depression + psychosis, or depression + anxiety + psychosis. Choosing to draw the borders around depression and say “Yup, this is the Actual Disease” isn’t a bad choice, but it doesn’t jump out of the data either. When people try to use sophisticated clustering algorithms on psychiatric disorders, they usually come up with something like this, where there are only three supercategories instead of the 297 different diagnoses in the DSM. And even three supercategories are pushing it – people with psychosis are far more likely to have depression too! Having any number of categories starts seeming arbitrary and fuzzy.
So Nuijten, Deserno, Cramer, and Borsboom (from here on: NDCB) ask: what if that’s wrong? What if there isn’t a latent variable like “influenza”? What if it’s symptoms all the way down?
Consider a network in which each symptom is a node, connected to all the others by pathways with certain weights on each direction. So for example, “sleep disturbance” might be connected to “fatigue” by a strong path – people with disturbed sleep are much more likely to be tired. These might both be connected to “low mood” – people who don’t sleep well, or who are tired all the time, start feeling down about themselves. And this path might go the other way too: people who feel down about themselves might have more trouble getting to sleep on time. And maybe all of these are connected to suicidality, because if you feel bad about yourself you’re more likely to commit suicide, and if you’re suicidal you might feel bad about it, and if you’re tired all the time then maybe you can’t accomplish anything useful with your life and so death might seem like a good way out, and so on.
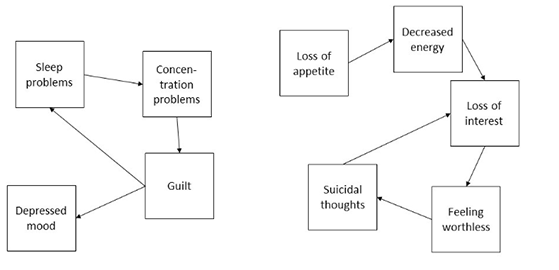
A sample image from the paper, showing two possible simple networks of depression symptoms
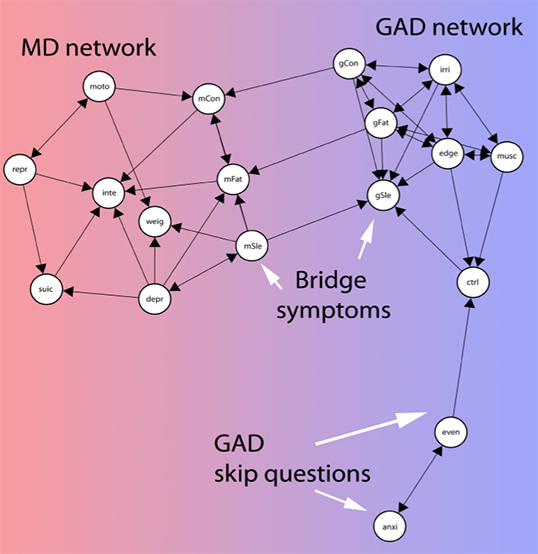
Also from the paper. This shows a more complicated (and apparently empirically validated) network of symptoms. MD is major depression. GAD is generalized anxiety disorder. The nodes are all different symptoms – for example, “inte” is “loss of interest in activities” and “musc” is “muscle tension”.
Not from the paper. But if you figure out a good way to calculate weights on this one, email me.
Each node might affect the others with a certain delay. Being suicidal might make you feel guilty, but even if your last suicidal thought was fifteen minutes ago, you might still feel guilty now. Maybe it would take months or even years before you no longer felt guilty about your suicidal thoughts. So there could be loops: in a simple model, your low mood makes you feel suicidal, your suicidality makes you feel guilty, and your guilt makes you have low mood. This type of loopy network might be stable and self-reinforcing. Maybe your boss yells at you at work, which makes you have a bad mood. Then even if the direct effect of your boss would go away quickly, if it causes suicidal thoughts which cause guilt which cause more low mood, then the cycle can stick around forever.
In NDCB’s model, all possible psychiatric symptoms are connected like this in a loose network. Particularly tight-knit symptom clusters that often active together and reinforce each other correspond to the well-known and well-delineated psychiatric diseases, like depression and schizophrenia. But there are no natural boundaries in the network; low mood and poor sleep may be closely connected to each other, but they’ll also be more distantly connected to anxiety, and even more distantly connected to psychosis. This corresponds to the fact that some depressed people will develop psychotic symptoms, even though psychosis isn’t usually associated with depression. The paths aren’t usually as strong as those between low mood and poor sleep, but they’re there, and in some people with a predisposition to psychosis or some idiosyncratic factor strengthening those paths beyond their usual level in the population, that will be enough.
There are lots of good things about thinking about psychiatric problems this way:
1. It helps explain how life stressors can cause depression. Some people who have a bad breakup will get depressed. This should be mysterious if we think of depression as a biological illness – and we have to at least a little; some people who take the drug interferon-alpha will get depressed afterwards too. But if depression is a symptom network, it becomes easier to explain. The bad breakup causes low mood, which under the right conditions and genetic predispositions can activate all of the other depression symptoms and create a stable, self-reinforcing depression. Likewise, poor sleep is a risk factor for the development of subsequent depression, which is hard to explain if we just think of it as a symptom of some latent-variable-style condition.
2. It explains how treating depression symptoms can treat the depression. I’ve heard a lot of different perspectives on this, but at least one of my attendings (and some studies) believes that treating poor sleep with a sleeping pill like Ambien can help dispel an underlying depression, including symptoms seemingly unrelated to sleep like “feelings of worthlessness and guilt”.
3. It explains how therapy can treat depression. If eg cognitive behavioral therapy helps you stop thinking of yourself as worthless, then you’ve de-activated the “feelings of worthlessness and guilt” node and made it a lot harder for all the other nodes to coalesce into a stable self-reinforcing pattern.
4. It explains the polygenic structure of mental illnesses. If a mental illness were one specific thing, we would expect it to have one specific cause, or at least be limited to genes active in one specific area or process. In fact, it’s hard to come up with anything that genes involved in these illnesses have in common other than “they’re mostly expressed in the brain” – and sometimes not even that. In NDBC’s model, genes might be involved in any of the symptoms, or in the paths between the symptoms. A gene involved in poor sleep could predispose to depression. So could a gene involved in low energy levels. Even a gene involved in anxiety or psychosis could have some effect. And so would any gene that influenced the probability that, given poor sleep, a person would have low energy levels; or that given anxiety, a person will have psychosis. The end result would be everyone having a slightly different network, with different amounts of work needed to activate each node and different weights on each of the inter-nodal paths.
5. It helps explain why so many brilliant people searching for The One True Cause Of Depression have come up empty.
II.
Actually, this last one deserves more explanation. NDCB think of these symptoms as visible patient complaints (“poor sleep”, “feelings of worthlessness”), and treat the connections between them as common sense (“if you don’t sleep, you’ll probably be fatigued”, “if you feel very guilty, you might attempt suicide because you think you deserve to die”). But their theory also works for networks of biological dysfunctions, or networks that combine biological dysfunctions with common-sense observed symptoms.
For example, we know that there’s a link between depression and inflammation. But it’s not a very good link; not all depressed people have increased inflammation, not all people with increased inflammation get depressed, and drugs that decrease inflammation don’t always cure depression. There’s similarly good evidence linking depression to folate metabolism, serotonergic neurotransmission, BDNF levels, and so on. Suppose we made a graph like the ones above, except that instead of putting things like “poor sleep” and “feelings of guilt” on it, we used “inflammatory dysfunction”, “folate metabolism dysfunction”, “serotonin dysfunction”, and “BDNF dysfunction”. There are a lot of reasons to expect these things to interconnect – for example, folate helps produce a cofactor necessary for serotonin synthesis, so any dysfunction in folate metabolism could make a problem with serotonergic neurotransmission more likely.
In a best case scenario we could merge the biological and psychological perspective, replacing “disturbed sleep” with “disturbance in the orexin and histamine systems that regulate sleep” and “tiredness” with “disturbance in the dopamine system that regulates goal-directed action”, and so “poor sleep makes you tired” with “disturbance in the orexin system causes a disturbance in the dopamine system”. In practice I expect this would be a terrible idea and that common-sense concepts mostly don’t have simple well-delineated biological equivalents. But what I’m saying is that the model where all of these things are observable symptoms, and the model where they’re all disturbances in brain chemicals and metabolism, aren’t necessarily in conflict.
So we can expand point (5) to say not only that it explains why nobody has found the One True Depression Cause, but why they have found so many promising leads that never quite pan out. Just like depression has a bunch of different symptoms, each of which is often-but-not-always involved, and each of which reinforces the others — so it has a bunch of different disturbances in biological systems, each of which is often-but-not-always involved, and each of which reinforces the others. Maybe there’s a nice correspondence between one disrupted biological system and one symptom, or maybe they sit uneasily together as different nodes on the same big graph.
III.
Are there any problems with this theory?
There are a couple of disorders that really don’t fit this model. Bipolar disorder, for example, doesn’t quite work as a collection of self-reinforcing symptoms. It’s marked by depressive episodes that can give way to years of stable mood before the person has a manic episode months or years later. I can’t think of any way to model this except as some underlying unified tendency toward bipolar disorder – although the ability for this tendency to cause a depression that looks just like normal unipolar depression is a point in NDCB’s favor, since it suggests there can be many different causes for the same syndrome.
The impressive success of ketamine also counts as a point against. NDCB imagine psychiatric disorders like depression as gradually fading out on a symptom-by-symptom basis, eventually reaching a point where enough symptoms are gone that the rest of them aren’t self-reinforcing and just sputter out. This matches the course of eg SSRI treatment, where the medications will gradually improve a few symptoms at at time over the space of a month or so and maybe cause a full remission if you’re lucky. It doesn’t really match ketamine, where every aspect of depression vanishes instantly, then returns after a week or so without treatment. There are a couple of other equally impressive things – staying awake for thirty hours straight, for example, can have an immediate and near-miraculous antidepressant effect, which unfortunately vanishes as soon as you go to sleep. Both of these treatments seem like direct strikes against the One True Cause Of Depression, and both suggest that an underlying tendency toward depression can exist separate from any symptoms (or else why would the depression come back after the effects of the ketamine wore off?)
I don’t think it’s possible to cure depression by blasting every symptom simultaneously. That is, suppose somebody is depressed with symptoms of poor sleep, poor appetite, low energy, suicidality, and low mood. Ambien can make them sleep. Pot can make them eat. Adderall can give them energy. Clozaril can make them stop wanting to kill themselves. And heroin can perk up mood. So if you gave someone Ambien, pot, Adderall, Clozaril, and heroin at the same time, would that cure their depression? I’m pretty sure no one has ever tried this, but I don’t think anyone’s reported exceptional results from less extreme cocktails like Adderall + trazodone + pot, which I’m sure a bunch of people end up taking. This along with the stuff from the last paragraph suggests that if we want to go with this model, maybe we should think less in terms of actual poor sleep and more in terms of dysfunction in the biological system of which sleep is a visible correlate. In that case we could say that Ambien helps the sleep itself but not the underlying dysfunction. But that takes some of the elegance out of the theory.
Despite these issues, I feel like something along these lines has to be true. There are too many things that sort of kind of cause psychiatric problems, and too few things that look like One True Causes. Things that look a lot like schizophrenia can be caused by viral infections in utero, by genetic factors, by hitting your head really hard as a child, by hypoxia during the birthing process, by something something something intestinal tract, by something relating to immigration which seems like it might involve psychosocial stress, and so on. Studies of the immune system, the dopamine system, the glutamate system, and the kynurenine system have all found disruptions. There have been so many really brilliant attempts to reduce all of these to a single brain region, or the levels of one specific chemical, or something that’s simple in the same way that lack-of-insulin-causes-diabetes is simple. But nobody’s ever succeeded. Maybe we should just give up.
I guess I’ve felt for a long time that some kind of weird change in attractor states of biological systems is the best way to explain these kinds of things, but I was never able to express what I meant coherently besides “weird change in attractor states of biological systems”. NDCB offer a clear model that suggests good avenues for future research.
(And I wasn’t joking when I said that little diagram with the two pentagons was the solution to 25% of extant philosophical problems.)














In a model of mental disorders as self-reinforcing networks, does electroshock therapy make more sense as a way to disrupt the network all at once?
It’s great to see something akin to control theory being applied to cognitive processes. I mean I have no training whatsoever in psychology and only the most superficial understanding of neuroscience. I’m an engineer. But if I squint at how the mind works I recognize lots of feedback loops.
* Confirmation bias reinforcing a stable set of predicates about the world (and other biases).
* When you think you may notice that some ruminations (or thought chains in general) keep returning to the same thoughts.
* In a dispute you may reach a state where anything you say makes it worse.
My private name for this is mental attractor. Some might just call it memes – ideas that propagate themselves – but I think that leaves out the interconnectedness of thoughts. These are self-reinforcing clusters like the symptoms mentioned.
The DSM on depression seems to list symptoms on a scale between the biological/physical (exhaustion, sleep) and the cognitive (suicidal ideation). I don’t understand anything about biology but it seems clear that there must be some link between how ideas are formed and bodily needs and function. Thoughts have a complex causal link to biology (call it symbol grounding).
So to me it seems that when (relatively stable) mental attractors coincide with/are grounded in (by whatever neuropsychological mechanism) endocrinological systems that make you tired, depressed (those more physical symptoms), then you have got a problem. Independent of how you arrived at that unlucky coincidence. And I guess it also works the other way around: Tiredness makes some thoughts more salient and thus the successor thoughts (there was a recent post about a study about mental states that I can’t find right now and I think that could be modeled as a parametric markov chain).
Anyway. It is nice to see that there is a theory that works on a level nearer to biochemical processes (which don’t really understand) which follows similar principles like that seen in more abstract cognitive processes.
A way in which bipolar disorder may fit into this model is if the network allows something akin to phase transitions to happen. If the effect of changes in the strength of neighbouring symptoms is high for a person (there are e.g. many connections in his network of symptoms and the thresholds for influence and multiplication factors are high), then a change in a single symptom could trigger all symptoms to become present much more. The underlying susceptibility is then the exact structure of their network of symptoms.
I doubt this is terribly informative since it’s pretty much pure impression and gut feeling but when I first saw those networks the first thing I thought of was gene expression networks. Gene A produces product B which suppresses or promotes gene C etc.
Sometimes A produces B which suppresses A.
One notable thing about gene expression networks is that there’s a surprisingly small number of stable configurations. A lot of the time if you push things too far out of whack they fall into self destruct apoptosis mode.
So the model makes intuitive sense though you might need more complex connections with both positive and negative effects.
it also makes sense that people can end up stuck in states where everything is reinforcing itself and anything which kicks them out of that has a good chance of helping.
Regarding bipolar disorder being different, I think you’d find it interesting that bivariate twin studies find that bipolar and “unipolar” depression are caused by different gentic factors. So my identical twin having bipolar disorder wouldn’t increase my probability of getting major depression that much. It would increase my schizophrenia risk though (lots of shared genetic variance)! (and then you compare this to siblings in an ACE model, you know the drill)
(Also a fun fact, Generalized Anxiety Disorder and major depression is pretty much genetically indistiguishable.)
(source: Plomins textbook on behavioral genetics).
“In a best case scenario we could merge the biological and psychological perspective”
As you later point out, sometimes the higher-order summaries of the symptoms might really be more useful in such a perspective. Interestingly to me, my girlfriend (clinical CBT psychologist who works on transdiagnostic stuff) pointed out that she feels a lot of cognitions could be added (e.g. certain thoughts cause guilt only if you have certain moral ideas saying they should cause guilt).
She also points out, that so many CBT models of psychological illness already involve positive feedback loops and vicious-circle-type ideas (even if the main analytic approach has been latent variables) that the main thing she found novel/was happy for someone saying out loud is that these loops of course aren’t limited to one illness/the comorbidity perspective. But she was also really excited about the personalised aspect of it.
Eiko, is there a paper from your group that explicitly relates network ideas to the concepts of vicious circles/positive feedback loops in common psychotherapy theory? The stuff I skim seems to focus more on the comorbidity perspective more (more novel?) but I’d love to see an explicit account of what y’all think of this, and it feels like it might help clinical people translate your stuff to the vocabulary they have.
I’d also be interested in how you decide which things to include in the network analyses. I saw an early talk by Denny (the one with “psychologists would be looking for the latent bird”) and I think that was “only” named DSM-4 symptoms?
This might be true but it’s so… unsatisfying. No cause, just a self-reinforcing loop of symptoms?
On the other hand, plenty of these conditions recur after being in remission for a while. So it seems there is likely some sort of attractor which makes the loop more likely to start. So we* can go looking for a cause for that.
*and by “we”, I mean definitely not me. People with lab coats and an endless supply of grad students.
I don’t know the math here well enough, but I was under the impression that stable attractors don’t need “causes”, at least not any more than “the relationships of the network produce this attractor”.
But the network is different for different people. Perhaps there is some reason some people’s networks have these nasty attractors, and perhaps the network can be changed somewhat, so (for instance) a temporary sleep problem isn’t going to result in a self-reinforcing loop of depression.
Right, but the “reason” could be as diffuse as “the distribution of connection weights in the network”. Which could be due to any number of co-occurring factors.
That being said, it’s also plausible that there are relatively discrete causes for some attractor states. But it’s equally plausible that for many of them, the cause is simply the total history of the network’s development, with no particular thing that stands out.
At least I think that’s true, however as I said my understanding of the math here is very hand-wavy, so anyone who knows what they’re talking about should correct me.
Random thoughts inspired by what you wrote here Nybbler…
I dunno how this might overlap or not with the network view, but is it not possible that something like depression has multiple contributing causes, in the same way cancer does?
We know Vit D deficiency, low thyroid, and a variety of other medical conditions can “cause” depression. It is plausible to me that subclinical problems with Vit D or hypothyroidism plus some other variable (bad relationship, stressful job, loss of a parent, some other medical condition) might together “cause” depression.
It seems to me the problem isn’t that there aren’t causes; it’s that the process of depression or anxiety is overdetermined. Once you add in personality factors, like perfectionism or black-and-white thinking or a vulnerability like trauma history, and social factors like poverty or isolation or situational stress, there are just a lot of possible contributing causes.
Insofar as depression or anxiety are defined only by clusters of symptoms (in the DSM), they are more like having a runny nose. The runny nose could be caused by allergies, a cold, the flu, weeping, inhaling dust, eating spicy food, or some combination of all of these. And yet understanding which caused them is very helpful for treating the runny nose. We just don’t know enough yet in psychology to tease apart all the potential causes. It doesn’t mean there aren’t any.
While the DSM doesn’t speak to causes at all, clinical folks have long been trained to look for multiple biological, social, psychological contributing factors, the mix of which is somewhat particular to each person and the correction of which often can resolve the anxiety or depression.
I wonder if what’s a “central” symptom in network terms (and therefore the place to focus treatment) varies considerably from one person to another, so that knowing what’s statistically the most common central symptom may not help too much in guiding individual treatment.
It makes sense to me to throw drugs (or other substances, like Vit D or methylfolate) at the biological “causes,” but that the other causal factors need to be addressed in their own domains, which is why therapy keeps turning up as equally useful as drugs.
“I dunno how this might overlap or not with the network view, but is it not possible that something like depression has multiple contributing causes, in the same way cancer does?”
Definitely. But the question from this perspective of symptom-based research would rather be: do specific depression symptoms have specific contributing causes? The answer is yes, they do (see also this paper).
“I wonder if what’s a “central” symptom in network terms (and therefore the place to focus treatment) varies considerably from one person to another, so that knowing what’s statistically the most common central symptom may not help too much in guiding individual treatment.”
You very quickly caught a core issue in the field: modeling individual people and their processes (idiographic modeling) vs modeling groups of people (nomothetic modeling).
We write in detail about this point in a overview and challenges paper to the network approach here (see chapter on heterogeneity pp. 25 here)
Thank you for the links and the reply, torvon. I’m excited to read more! Very glad for the work you all are doing.
As noted in one of the links, there are three, or maybe even one, underlying factors. So it may be that there’s an underlying p-factor, or an underlying depression factor which makes you more prone to falling into a depression loop, but anyone can fall into one given the right stimulus, you just have less of a barrier to it.
Just because there is no cause doesn’t mean that there aren’t things which might feed into it or make you more susceptible.
It might also be that having multiple weak nodes that feed together could keep generating loops even after you broke one.
Huh, I gotta admit, I found this article pretty surprising. I am not a scientist, but I work in bioinformatics; and in this field, pathway networks like the ones Scott is describing are old news (*). Everyone knows that genes are not blueprints, so if you want to understand the relationship between the genotype (i.e. DNA) and the phenotype (e.g. how tall a person is), you need to study these pathways, in aggregate. Psychiatry is at least as complicated as biology; you’re telling me that no one had come up with this idea until now ?
I know I’m speaking from ignorance, but still, it just sounds weird… Is psychiatry scientific at all ?
(*) Note that this is a chemical pathway, not a gene expression pathway, but the idea is similar. Also, TIL there exists an animal known as the “crab-eating macaque”.
I didn’t! Well, not really. How do they compare to Kernel/Machine level computer code? Do you by any chance have a link to any good explanation of how genes are conceptually different from (or similar to) low-level programming?
I’m not sure if you’re being sarcastic or not, so I’ll take you at your word. FWIW, biologists tend to cringe when people tell them (usually, excitedly) that genes are totally like binary code.
Anyway, one place to start would be the Wikipedia article on gene expression, as well as the article I linked above to gene expression pathways.
Generally speaking, genes are chemicals, not computer code. This means that all of their behaviours are stochastic. While it is generally true that a specific gene will produce a specific protein, it will not do so 100% of the time. Genes can be “expressed” — meaning, actively working to produce proteins — with varying strengths (i.e., the probability that this gene will actually produce a protein). Furthermore, many (if not most) genes have alternative splicing forms, where the same string of DNA will produce a slightly different protein, depending on the chemical conditions within the cell.
What makes things more complicated is that many of these proteins act as parts in the cell machinery that turns more genes into more proteins. So, if gene A produces protein A1, and that protein suppresses the work of gene B that produces the protein B1, but B1 enables gene C to produce proteins C1 and C2, where C1 regulates A and C2 regulates D… then what happens ? The answer usually is some kind of a massive pathway graph, with conditional probabilities attached to each edge.
To be fair, there are a few genes that appear to regulate a single trait; but such genes are very rare. For example, Monsanto got very lucky and found their “Roundup-Ready” gene, which makes corn immune to a specific type of herbicide. So, now they can blast the field with that herbicide, and everything in it will die, except for Monsanto corn. That’s great, but Monsanto sank billions of dollars into R&D since then, and so far they have not been able to come up with anything nearly as definitive (AFAIK, anyway).
So, in summary, genes are not computer code at all. Some aspects of their behavior are very similar, but in general their behaviour is probabilistic and, as of yet, poorly understood.
Wasn’t being sarcastic. Thanks, I appreciate the explanation.
Edit: This probabilistic vs. deterministic difference seems like part of a larger composed vs. block structure: Computer operating systems are planned in blocks (as such), because they need to be simple enough for human programmers to understand. Biological systems don’t (and I suspect being in blocks would be actively harmful, since then random mutation would be much more likely to be harmful vs. beneficial).
One fundamental block is error correction – computers can have bits randomly go wrong, so the low-level blocks have error correction built in, and we can treat the bits as deterministic. A biological system wouldn’t be constrained by wanting to think things out in terms of bits, and could have a large random structure with the “error correction” (that is, ensuring minor chemistry variations on the cellular level don’t kill you) on a macro scale.
… In general, biological engineering is awesome. It’s a shame it’s probably too complicated for any human to fully grok. I’m frankly amazed Monsanto ever got as far as they did.
Actually, there’s quite a bit of error correction as well as redundancy built into the DNA machinery. For example, several different codons (groups of 3 nucleotides, the building blocks of DNA) code for the same aminoacids (the building blocks of proteins); this makes it possible for a mutation to occur without changing the organism at all. There’s also stuff like Nonsense-Mediated Decay which performs a similar function to a CRC check. There are other mechanisms, too, but fortunately they are not perfect — or else evolution wouldn’t work.
In addition, as far as I understand, there are distinct subsystems within DNA, as well; in fact, this is why we can study gene expression networks as semi-distinct items at all — otherwise, it’d all be one giant undifferentiated graph. What’s more, you can often trace the line of descent of an organism by following huge pieces of its DNA as it made its way into its descendants (or, more likely, by looking at siblings on the phylogenetic tree). For example, the 1st chromosome of Rice is pretty much the same as the 3rd chromosome of Sorghum, with a couple pieces reversed.
In general, biology is definitely too complicated for any human to fully understand; but then, so is electronics. I doubt there’s a single human being on Earth who fully understands how a modern computer functions, from the quantum level all the way up. That’s not really a problem though — we humans are social animals, after all.
Furthermore, AFAICT biology had received a huge boost in productivity lately, due to the advances in machine learning, and processing capacity in general. The first Human Genome Project cost a billion dollars (or thereabouts); today, you can fully sequence a person’s DNA for about $100,000, and the prices may be coming down to $10,000 soon. On the analysis side of things, right now I could click a button and spin up a 1000-CPU cluster on Amazon, to analyze my 100 TB of data. This is the kind of power that would give Watson and Crick continuous earth-shattering science-gasms for years 🙂
Great, now I’m imagining Watson and Crick having sex with a giant computer.
FYI, finding resistance genes is relatively easy but something of a matter of luck; if you dump a bunch of poison or antibiotic on something, and then breed the survivors, then dump more poison, ect. you can isolate a population which is resistant and then look for the gene.
The problem is it is a matter of luck as to whether or not you have any resistant members of your population in the first place, and whether one or multiple genes are involved in resistance, and whether they have deletorious effects otherwise (a lot of antibiotic resistance genes in bacteria, for instance, also make the bacteria worse at reproducing).
For example, Monsanto got very lucky and found their “Roundup-Ready” gene, which makes corn immune to a specific type of herbicide. So, now they can blast the field with that herbicide, and everything in it will die, except for Monsanto corn.
Going off at a tangent here, but that is part of the reason I’m very wary about the enthusiasm for monoculture of GMO crops as the solution to world hunger or whatever. As in the example above, this works great in the field as long as blasting the herbicide does kill everything but the GMO corn that is resistant to it.
But unfortunately, there is this little matter of herbicide resistance since in the field is not in the controlled condidtions of the lab, and plants can develop tolerance, including glyphosate tolerance which is what Roundup is, and there is the prospect of having your advantage in growing GMO corn that can survive blasting with herbicide fading when the weeds catch up. Which is why there are guidelines about reducing the chances of glyphosate resistance, just as with antibiotic resistance. It’s no longer the case that Roundup can reliably kill everything, so just spray the hell out of your fields.
And as you point out, Monsanto got lucky with that one gene, but there isn’t anything else on the horizon that’s similar (as of yet). So putting all your eggs into one GMO basket is not the magic bullet (to mix a metaphor).
The irony of advice about using the old-fashioned, labour-intensive methods of controlling weeds to avoid herbicide resistance developing (as below), as would be the case in the developing world countries where GMO crops and their attendant herbicide reliance are touted as the modern, progressive, technological solution to the food production problems of these countries is not lost on me:
For every Monsanto, there’s a Norman Borlaug. In the grand scheme of things, given the number of people who are alive on the planet today, and factoring in population growth, I don’t think it’s even remotely possible to feed everyone just by sticking to “old-fashioned, labour-intensive methods”. We need genetically engineered crops, and the question is, “how can we implement them safely”, not “how can we get rid of GMOs”. Monsanto probably doesn’t care about herbicide over-use, but that’s a problem with Monsanto, not with their corn.
By the way, as far as I understand, most (if not all !) of our modern crops are genetically engineered — except that most of that engneering took pace over thousands of years, using very inefficient processes. Some of our crops, like corn, are also transgenic. This part is new, but that doesn’t make non-transgenic corn somehow fully natural. Compared to wild-type grains, it’s still a hideous abomination.
I was under the impression that in general fields got ‘less scientific’ as they got more complex. Complexity meaning it is harder to do controled experiments and simple models etc. I don’t actually study any field, so this could be totally wrong?
Math
Physics
Chemistry
Biology
Etc
You are probably right, but then why have psychiatrists been working on simple models until now ? Seems like they should know better — though again, I’m pretty ignorant about all of this, so I could be wrong…
I don’t know much about psychiatry, but I’m working in cognitive neuroscience / psychology, and we’re just beginning to move towards truly sophisticated models. I think the main reason is simply that until about 30 years ago, there was very little data about brain function, and the types of data we did have were piecemeal and disconnected from each other. It turns out the brain is really complex, and also really hard to observe in action, and we haven’t been doing it very long.
Most psychiatrists, if I understand correctly, don’t do research at all, so the problem is even worse there.
I don’t think those fields become less scientific necessarily, but the people doing research in them have to become hyper-specialized in one sub-sub-sub-sub research area just to be able to grok all the current knowledge and make forward progress.
Semi-related: In Asimov’s foundation series, he came up with two models for how psychohistory worked throughout the series. The first (in the original trilogy, written when he was young), had it based on modeling basic brain interactions and working your way up.
The second, in the prequel books (about Hari Seldon’s life, written when Asimov was much older), Seldon bases his theory on looking at history and building mathematical models to predict it.
‘m not sure what caused the change – could be that talking about looking at history made for a better story once he was trying to write a story from Seldon’s perspective, but it’s also possible that after he gained more science experience Asimov realized the notion of building a model from the ground up was too unbelievable, and went for a more realistic model.
They aren’t less scientific.
First off, math isn’t a science in the first place; it’s a form of logic. Math is useful, but it isn’t scientific at all.
Physics, chemistry, and biology are all “hard sciences”, as are some others. All three allow for experimentation, not just observation; you can actively run experiments and get results in these fields.
Biology is actually quite scientific, but it is also really, really hard. The core area of biology is quite solid, with it getting more questionable as you go out towards the periphery. That said, biology is not “complete”. Then again, neither are chemistry or physics; protein folding is a chemical problem underlying a lot of biology, and it is far from solved. In fact, a lot of low-level biology comes down to chemistry. That said, there’s a lot of emergent complexity in biology.
If you look at biology and compare it to physics, biology is often more qualitative rather than quantitative. But a lot of biology is statistical in nature.
@Bugmaster — as a biophysicist, I felt exactly the same way. Isn’t it obvious that one has to consider networks, pathways, etc., in a complex system? In fairness, I suppose, many biologists, despite knowing this, insist on studying what one gene “does,” so this is apparently a hard lesson to internalize. Plus, biology has the advantage over psychology that a lot of interaction networks are at least somewhat known, in enough detail to be modeled, which makes their importance more obvious.
This post reminds me of the ‘Functional Medicine’ approach applied to psychiatry. Seeing things as as multiple symptoms and systems that interlock in ways unique to each patient rather than ‘diagnosis—>standardized treatment’ systems more common in medicine.
(the reason why that is the standard model actually has a lot to do with that ‘Big Macs vs. the Naked Chef article you linked recently; it mechanizes healthcare so that more people can do it. It also makes it easier for medicine to interact with insurance.)
The result is treatment modalities that try to treat disparate parts of the pathology simultaneously, and an emphasis at treating suspected root causes (which may not always be intuitive).
Unfortunately functional medicine, as with a lot of counter-establishment things, is a bit of a lightning rod for radicals and loonies and so suffers from an, uh, image issue. The Wikipedia page is a hit piece. But the conferences I’ve attended more recently involving people like the Institute for Functional Medicine have had a pretty high standard for scientific inquiry and evidence, and I see it converging with more mainstream medical beliefs. 15-ish years ago it was (mostly) herbs and homeopathy, now they still keep some of the herbs but also talk about integrating them with more conventional approaches. And to be fair, their ideas about some of the herbs and supplements have been validated to a degree. And the ones that work tend to be gentler agents than isolated-compound pharmacology which makes them better-suited to tweaking smaller background issues.
This is pure speculation. On bipolar disorder, could the nodes be changes in emotional feedback mechanisms?
When someone gets sad, there are some positive feedback loops. Ex. Get sad. Mope rather than doing fun things. Get sadder. Listen to sad music. Get sadder. etc. There are also negative feedback mechanisms. Get sad. Go to sleep and wake up. Be less sad. Do a fun activity you previously scheduled. Be less sad. For happiness to manic there are also both positive and negative feedback mechanisms.
Are there common feedback mechanisms to both? Because if they are, then the nodes for manic and depressive episodes might be the same, but work differently in each case. “Increased change in activity based on mood” could make someone who is happy become happier and someone who is sad become sadder. “Slower regression to mean mood” could make depressive and manic feedback loops more likely to run out of control.
extremely tangentially related (I’m mostly writing this out because I want to get my thinking down in words, ie https://news.ycombinator.com/item?id=13158364)
—————
“4. It explains the polygenic structure of mental illnesses. If a mental illness were one specific thing, we would expect it to have one specific cause, or at least be limited to genes active in one specific area or process. In fact, it’s hard to come up with anything that genes involved in these illnesses have in common other than “they’re mostly expressed in the brain” – and sometimes not even that. In NDBC’s model, genes might be involved in any of the symptoms, or in the paths between the symptoms. A gene involved in poor sleep could predispose to depression. So could a gene involved in low energy levels. Even a gene involved in anxiety or psychosis could have some effect. And so would any gene that influenced the probability that, given poor sleep, a person would have low energy levels; or that given anxiety, a person will have psychosis. The end result would be everyone having a slightly different network, with different amounts of work needed to activate each node and different weights on each of the inter-nodal paths.
5. It helps explain why so many brilliant people searching for The One True Cause Of Depression have come up empty. ”
is really interesting, and is interesting to think how many things work like this, and what are ability to model things that work like this is
couple post again, I had this discussion: https://slatestarcodex.com/2016/12/06/links-1216-site-makes-right/#comment-442210
about whether the world is getting easier or harder to model
and today read this article (which is an excerpt from Michael Lewis’s upcoming book) : http://www.slate.com/articles/arts/books/2016/12/how_daryl_morey_used_behavioral_economics_to_revolutionize_the_art_of_nba.html
which is about, among other things, the difficulties of creating models to predict basketball players
excerpt of the excerpt:
Morey could see—or thought he could see—how the model had been fooled by Joey Dorsey. Its blindness to the value of DeAndre Jordan was far more troubling. The kid had played a single year of college basketball, not very effectively. It turned out that he had been a sensational high school player, had hated his college coach, and didn’t even want to be in school. How could any model predict the future of a player who had intentionally failed? It was impossible to see Jordan’s future in his college stats, and, at the time, there were no useful high school basketball statistics. So long as it relied almost exclusively on performance statistics, the model would always miss DeAndre Jordan. The only way to see him, it seemed, was with the eyes of an old-fashioned basketball expert. As it happens, Jordan had grown up in Houston under the eyes of Rockets scouts, and one of those scouts had wanted to draft him on the strength of what appeared to him undeniable physical talent. One of his scouts had seen what his model had missed!
Morey—being Morey—had actually tested whether there were any patterns in the predictions made by his staff. He’d hired most of them and thought they were great, and yet there was no evidence any one of them was any better than the other, or the market, at predicting who would make it in the NBA and who would not. If there was any such thing as a basketball expert who could identify future NBA talent, he hadn’t found him. He certainly didn’t think that he was one. “Weighting my personal intuition more heavily did not cross my mind,” he said. “I trust my gut very low. I just think there’s a lot of evidence that gut instincts aren’t very good.”
In the end, he decided that the Rockets needed to reduce to data, and subject to analysis, a lot of stuff that had never before been seriously analyzed: physical traits. They needed to know not just how high a player jumped but how quickly he left the earth—how fast his muscles took him into the air. They needed to measure not just the speed of the player but the quickness of his first two steps. That is, they needed to be even more geeky than they already were. “When things go wrong, that’s what people do,” said Morey. “They go back to the habits that succeeded in the past. My thing was: Let’s go back to first principles. If these physical tools are going to matter, let’s test them more rigorously than they’ve ever been tested before. The weights we placed on production in college had to go down, and the weights we placed on raw physical abilities had to go up.”
But once you started to talk about a guy’s body and what it might or might not be able to do on an NBA court, there was a limit to the usefulness of even the objective, measurable information. You needed, or seemed to need, experts to look at the tools in action and judge how well they would function playing a different game, against better competition. You needed scouts to rate a player’s ability to do the various things they knew were most important to do on a basketball court: shooting, finishing, getting to the rim, offensive rebounding, and so on. You needed experts. The limits of any model invited human judgment back into the decision-making process—whether it helped or not.
And thus began a process of Morey trying as hard as he’d ever tried at anything in his life to blend subjective human judgment with his model. The trick wasn’t just to build a better model. It was to listen both to it and to the scouts at the same time. “You have to figure out what the model is good and bad at, and what humans are good and bad at,” said Morey. Humans sometimes had access to information that the model did not, for instance. Models were bad at knowing that DeAndre Jordan sucked his freshman year in college because he wasn’t trying. Humans were bad at . . . well, that was the subject Daryl Morey now needed to study more directly.
Freshly exposed to the human mind, Morey couldn’t help but notice how strangely it operated. When it opened itself to information that might be useful in evaluating an amateur basketball player, it also opened itself to being fooled by the very illusions that had made the model such a valuable tool in the first place. For instance, in the 2007 draft there had been a player his model really liked: Marc Gasol. Gasol was twenty-two years old, a seven-foot-one center playing in Europe. The scouts had found a photograph of him shirtless. He was pudgy and baby-faced and had these jiggly pecs. The Rockets staff had given Marc Gasol a nickname: Man Boobs. Man Boobs this and Man Boobs that. “That was my first draft in charge and I wasn’t so brave,” said Morey. He allowed the general ridicule of Marc Gasol’s body to drown out his model’s optimism about Gasol’s basketball future, and so instead of arguing with his staff, he watched the Memphis Grizzlies take Gasol with the 48th pick of the draft. The odds of getting an All-Star with the 48th pick in the draft were well below one in a hundred. The 48th pick of the draft basically never even yielded a useful NBA bench player, but already Marc Gasol was proving to be a giant exception. (Gasol became a two-time All-Star in 2012 and 2015 and, by Houston’s reckoning, the third-best pick made by the entire NBA over the past decade, after Kevin Durant and Blake Griffin.) The label they’d stuck on him clearly had affected how they valued him: names mattered. “I made a new rule right then,” said Morey. “I banned nicknames.”
————-
————-
Couple of thoughts – I’m not sure I buy the ‘Morey is reinventing the paradigm’ narrative that Lewis is telling here, although I do think he’s doing a good job of not pitching that narrative too strongly and does do a good job of reflecting how difficult it is to build useful models, that don’t break under the stress of competition
back to your post, its seems like one of the difficulties building these models is that the work, is that (to stay the realm of predicting basketball players) the things you’re trying to predict, are an endless knot of traits, not whole entities in and of themselves
DeAndre Jordan – the excerpt makes that out like the model just missed him because the model didn’t account for his flakiness during his 1 year of college (or I guess actually overaccounted for it), but there were 32 different unique situations he could have wound up in, its possible that if he’d had different coaches, or different teammates, (or had a different girlfriend) those traits would have actually prevented him from succeeding
Lewis’ books (I’m counting this excerpt and Moneyball here especially) make it seem like the humans are just one cognitive error after another, screwing up all the decisions
but maybe that’s not the right way to look at we, we all have a pretty good supercomputer on top of our heads, programmed with millions of years of evolutionary code
maybe we’re better at figuring out how these complex things interact with each other than we give our selves credit for
————–
————–
sorry about relating everything to sports, that just how my brain functions
Something that seems important, but which is left out in both the paper and your write-up is the possibility of a temporal component. For instance, what if there are not only links between nodes of varying strength, but also “activation thresholds”, “activation durations” and “relaxation times” for each node, based on underlying biology. Thus, our spouses both break up with us, setting off the links in the chain, but I have faster relaxation times in certain nodes, which causes various symptoms to die out too fast to ever form a stable cluster, while in you they persist and self-reinforce (an attractor). Bipolar could be what’s called a “limit cycle”, a stable periodic orbit through mathematical space, with the varying temporal components and connections determining the frequency. The consequences of ketamine and sleep deprivation would work too – after temporary removal of the patterns due to altering the dynamics of the nodes, the nodes reset to their original values and will once again converge on the attractor.
More visually, I’m imagining the network diagram for certain illnesses not as a static picture with certain nodes highlighted, but a video, where clusters of “lighted up” interacting nodes make ripples, pulses, waves, swirls, etc. over time, and just like how you can send a heart into and out of fibrillation with a stimulus at a precise place and timing (while other stimuli are erased quickly), life events can trigger pattern changes depending upon both the node stimulated *and* the timing relative to any existing patterns.
“More visually, I’m imagining the network diagram for certain illnesses not as a static picture with certain nodes highlighted, but a video, where clusters of “lighted up” interacting nodes make ripples, pulses, waves, swirls, etc. over time …”
These videos exist — there is actually plenty of methodological work happening on estimating such changing dynamics.
e.g.:
* https://www.ncbi.nlm.nih.gov/pubmed/27668421
* https://arxiv.org/abs/1510.06871
We talk about this in great detail in a new non-technical paper at:
* https://osf.io/vqsa4/
So, a bit of artificially-binary thinking on this:
Suppose we divide nodes over two axes – “receives feedback/doesn’t receive feedback from other nodes” (F/!F) and “produces/doesn’t produce noticeable symptoms” (S/!S). That is:
FS: receives feedback from other nodes, also produces symptoms. Drugs that target this node we would expect to suppress symptoms until you stop taking them, at which point symptoms return – e.g., your Ketamine example.
!FS: Produces symptoms, but doesn’t receive feedback from other nodes. Drugs here cure things right away, e.g., antibiotics for the not-yet-resistant bacterial infections.
F!S: Receives feedback, produces no symptoms itself. In the unlikely event you have drugs targeted here, their effects will be slow to start and quick to vanish if your patient is, say, less than diligent about taking them.
!F!S: No symptoms, no feedback. Slow, but relatively permanent changes.
The main thing is that feedback loops are not necessarily symmetric.
Why shouldn’t there be latent variables in these networks also?
How does this differ from the case of biological illness before the discovery of bacteria and viruses?
There we also had vague clusters of symptoms (based on the humors, or based on torpor, temperature etc..). There it also seemed like one could treat the disease by treating the symptoms. Get really sick and you get tired…sleep more and you get well faster. Sickness also stops people from keeping food down or raises their temperature too high..again remove these obstacles by treating symptoms and people get better.
The lesson I take from this is that there is only a limited amount that pure correlational analysis of outcomes can accomplish. The picture is only resolved by investigating theoretical causal properties (germ theory of disease) and then using those to reclassify all the information. We just haven’t done it for psychiatric problems yet.
—
While giving adderall+heroin+pot might be uncommon substitute subutex or methadone for heroin and it’s much more common.
Also, the reason these combos don’t tend to work isn’t because the depression isn’t treated but because those substances, especially in combination, often create their own issues that undermine any benefits. Develop drugs like these with less side effects (the adderall version of subutex) and I think you might see something different.
This is different, if I understand correctly, in that there may no underlying cause. The symptoms, and their interactions, are the problem.
One cool thing about this model is that it seems falsifiable.
If one weren’t depressed but knew that there was a risk of becoming depressed, would a viable preventative strategy be to just consistently keep an even strain on proactively addressing all of the possible symptom categories?
For instance, if you meditate, work out, force yourself to eat consistent meals, practice healthy self-esteem-promoting thought patterns, strive for stoicism in your personal interactions, keter, and get regular massages, would that effectively screen off any possibility of getting depressed? Or is there some ur-knob in your brain that can get tweaked regardless and make you depressed despite your perfect lifestyle?
This is social rhythms therapy for bipolar disorder (or maybe another therapy for bipolar disorder, I can never keep the names straight). It works well for many people, but I’m reluctant to use it on its own because it’s hard to predict who it won’t work for, and slip-ups can be really costly.
Costly in what way – just in possibly delaying other treatments? It seems like most of these tactics would be good things to do anyway.
One of the problems in how it fails if it isn’t effective. If a particular person would simply be tired if their depression wasn’t completely managed by social rhythms therapy the down-sides might be safe, if unpleasant.
The problem is that sometimes the failures involve self-destructive behaviour. I’ve personally seen the results of manic phases, severe depression, and somebody with (we think) schizophrenia. In these cases failure means actions which can or have lead to death. Nobody is going to want to take that risk when it’s uncertain if the fall-off curve is convex or concave. Drugs are much more certain in that case.
“One cool thing about this model is that it seems falsifiable.”
Absolutely — if depression really arises from mutual interactions, intervening on especially *central* symptoms or problems should alleviate other problems. If there is a common cause behind all symptoms (e.g. a brain disorder), then you’d need to target this common cause — treating a single symptom will do very little for the patient.
The p-factor is interesting, and it wouldn’t surprise me if it was genetic.
More problematic, however, is if there are actually two things – there’s both a symptom loop and an underlying genetic disorder which can both lead to depression/anxiety/psychosis/ect. If there are both, then it could be very hard to really isolate it.
The p-factor is not a reflective latent variable, but a formative latent variable. The positive manifold is true, but it does not necessitate a reflective factor.
For intelligence, this has been shown here very well. For psychopathology, I hypothesize that the same holds.
van der Maas, H. L. J. et al. A dynamical model of general intelligence: the positive manifold of intelligence by mutualism. Psychol. Rev. 113, 842–61 (2006).
There may be a distinction between bipolar disorder (and things like schizophrenia, etc.) and less severe disorders like depression or anxiety in that the former are genuinely defective systems (some genetic trait is missing like a neuro-transmitter or receptor) and the latter are instances of a functioning system (or less severely disabled) that is caught in a negative feedback loop. Conceptually, treating the symptoms of depression in this model could knock the system back into place, whereas with the bipolar model in would require more constant treatment as the system is incapable of self-regulation.
Just speculation based on your post.
I really like the network approach. Is there more information on this or is it that new?
Concerning bi-polar disorder. DSM V created some new diagnosis partly in response to too many people (kids maybe?) being diagnosed with bipolar disorder incorrectly. I think that should make us skeptical about the veracity of the bipolar data because there is high likelihood that there were treatments for bipolar that never were bipolar.
Psychiatrist Bessel van der Kolk suspects that quite a few people with a bipolar diagnosis, really have some kind of trauma disorder (PTSD, complex trauma, developmental trauma, etc…).
http://www.traumacenter.org/products/pdf_files/Preprint_Dev_Trauma_Disorder.pdf
Additionally, lithium has been found useful in treating PTSD symptoms.
https://www.ncbi.nlm.nih.gov/pubmed/7712052
This means that it’s not far fetched that an incorrect bipolar diagnosis was given but with a suitable treatment. The patient gets better and we are then convinced that the diagnosis was correct, even thought it wasn’t.
“I really like the network approach. Is there more information on this or is it that new?”
Plenty of information, papers, and tutorials at psych-networks.com !
And to think I thought depression was caused by conflicting control systems and higher levels that have yet to be reorganized. Oh well.
Is there any test where your model and the NDCB model would give different results?
Hi Callum G,
Thanks for the question. (:
I can link you a page with studies:
http://www.methodoflevels.com.au/about-mol/
Another study:
https://nextlevelstudy.wordpress.com/
More studies:
http://mindreadings.com/
A free book:
https://books.google.ca/books?printsec=frontcover&id=Da9lPEDayPMC&redir_esc=y&hl=en#v=onepage&q&f=false
A free study:
http://www.cambridge.org.secure.sci-hub.cc/core/journals/the-cognitive-behaviour-therapist/article/div-classtitlewhatandaposs-therapeutic-about-the-therapeutic-relationship-a-hypothesis-for-practice-informed-by-perceptual-control-theorydiv/98CF8D06E5A621F162361D3C2D1AEDBD
Another free study:
http://sci-hub.cc/doi/10.1017/S1754470X09990134
A test could be to see if one model outperforms the other in treating a patient. If they both work equally as well it means that its really some common process by which people with psychological issues get better. There are certain core process in getting better psychologically that M.O.L has claimed to discover. We could perhaps see if these universal process are truly universal processes.
The creator of the psychotherapy, Dr. Tim Carey, could be contacted here. He could answer any questions much better than me (i’m sure he will answer back).
http://www.methodoflevels.com.au/contact/
For some more general stuff related to the Method Of Levels:
pctweb.org
Hi agian Callum G,
You should also check out:
https://en.m.wikipedia.org/wiki/Common_factors_theory
https://en.m.wikipedia.org/wiki/Dodo_bird_verdict
Finally here is debate with a M.O.L researcher (look at the comments):
http://psychsciencenotes.blogspot.ca/2016/01/a-quick-review-and-analysis-of.html?m=1
Everything ive linked should give a great overview of PCT and MOL. This should help explain how and why a person gets better from a MOL perspective.
Thanks for the time.
As someone with no experience with psychiatry, but a lot of general analytic experience, this is kindof how I always assumed psychiatry viewed things. A lot of complicated nodes that can reinforce or dampen each other, and all the DSM labels are just useful categories for common kinda-similar clusters of behavior. When reading your article I was actually surprised to learn the NDCB model isn’t the standard view. Thanks!
I’m studying clinical psychology, and this is conceptually how clinical psychology views things. “Loops of symptoms” isn’t anything new, and loops of symptoms being responsible for common comorbidities isn’t new either. All of psychiatric illness is one big network is new though, I guess.
“Loops of symptoms” isn’t anything new, and loops of symptoms being responsible for common comorbidities isn’t new either.”
The new thing about the network approach to psychopathology is that new psychometric models were developed and implemented that allow for the estimation of these processes in dynamical systems. That’s a major step forward, and started with the Comorbidity paper by Angelique Cramer in 2010 published in BSS.
Torvon:
Interesting. Thanks 🙂 was genuinely confused about what the hype is here.
Fantastic blog, thanks for the great intro.
For folks interested in some further reading, we have a new paper in which we summarize the current empirical literature in this field (open access PDF). We’ve also set up a new website where we blog about new papers and developments in the field, and have a list of tutorials for researchers interested to get into network modeling.
There is also a new Facebook group on dynamical systems in psychology that is worth checking out.
Cheers
Eiko Fried, University of Amsterdam
Awesome resources, Cheers!
It’s there an accessible version of your full symptom graph? I poked around for a while and couldn’t find one.
“It’s there an accessible version of your full symptom graph? I poked around for a while and couldn’t find one”
Sorry, I’m not quite sure what you mean. Happy to help if I can.
> I don’t think anyone’s reported exceptional results from less extreme cocktails like Adderall + trazodone + pot, which I’m sure a bunch of people end up taking.
People abused Ketamine for decades, got the very impressive antidepressant effect and didn’t report it. Or maybe they did, but nobody believed them. (And quite a number of those Ketamine abusers were in fact doctors.)
And what about MDMA? It works really really well against PTSD, it has been in widespread use since the eighties and still three decades went by until the news started to reach the medical establishment.
I think that in the context of what illegal drugs do to the psyche (beyond basic pharmacokinetics), it is just really hard to separate the signal from the noise. Even if you believe users when they say they’re self-medicating, it can be hard to know whether they’re medicating mental disorders, withdrawal symptoms or lingering effects of previous overdoses. And then they all take different combinations of different doses of dubious quality substances.
tl/dr: If Adderall + trazodone + pot was as great for GAD as Ketamine is for depression, we’d still be unlikely to know.
MDMA was researched for its anti-psychotic properties before it was banned. I’m not sure where you got the idea that no one had heard about it.
Ketamine is a powerful drug; I’m not surprised no one had really researched it’s ability to fight depression. A lot of recreational substances are claimed to help with such; it would require an actual organized study to actually prove it, and you’re dosing people with ketamine, which is… well, a powerful drug.
RE bipolar, I think it is explainable by this model, but you have to look at the evolution of the influences in time. I can imagine a self-reinforcing loop in one set of nodes slowly reaching a threshold, after which another set of nodes get activated, which de-emphasizes the original set. After a while, that second loop reaches its threshold, switching the system back to the first loop.
Basically, an oscilation pattern in the graph.
Right, that’s a more precise version of what I was just groping to articulate.
I know very little about any of these issues, but Scott’s comment about bipolar not being explainable by the new model made me wonder. First factual question: if I have bipolar disorder, do I always swing from depressive episodes to manic episodes and vice versa (with “normal” episodes in between)? Or does the chain sometimes go depressive-normal-depressive and manic-normal-manic?
Because if the latter is the case, it seems to me that you can just imagine a system such as described here with two stable attractors instead of one. If it only swings in particular directions, it’s harder to do that, although there may well be systems with two attractors that work that way.
Bipolar II, will frequently feature depressive-normal-depressive shifts as well as depressive-normal-hypomanic. Not sure about bipolar I; IIRC the episodes tend to be more severe but less frequent. With type II, depressive episodes (mild and severe ones) are common, and hypomania usually doesn’t occur as frequently for the person nor last as long. There’s no mania, of course, because that’s the difference between the types: type I includes full-blown mania and type II doesn’t.
Being suicidal might make you feel guilty, but even if your last suicidal thought was fifteen minutes ago, you might still feel guilty now. Maybe it would take months or even years before you no longer felt guilty about your suicidal thoughts. So there could be loops: in a simple model, your low mood makes you feel suicidal, your suicidality makes you feel guilty, and your guilt makes you have low mood. This type of loopy network might be stable and self-reinforcing. Maybe your boss yells at you at work, which makes you have a bad mood. Then even if the direct effect of your boss would go away quickly, if it causes suicidal thoughts which cause guilt which cause more low mood, then the cycle can stick around forever.
Speaking from the symptoms side of the fence, it doesn’t quite work like this (or at least, not from the one case I can tell you semi-reliably about, which is my own). This is also probably why CBT did nothing for me, because it’s predicated on this kind of “treat behaviours” model, where it goes “Aha! See, by doing some thinking, you realised that your suicidal thoughts are caused by your guilt which is caused by your bad mood when your boss yelled at you, so let’s see how we can help you cope with being yelled at by your boss” and that helps because “behaviour influences thoughts and thoughts influence behaviour”.
But when there aren’t handy little triggers like this – there is no ‘my boss yelled at me so that’s why I’m feeling low’ explanation – it’s not so effective.
And that’s why even though I had no problems at work, got on with my colleagues and superiors, and wasn’t having difficulties coping, hated the work, or had people yelling at me, I still ended up in the mornings crying in the bathroom at work because I felt so wretched. Low moods and suicidality are the background to everything, not “oh this happened so that sparked it off”. Unless you can figure out some huge major cause that happened to me between the ages of ten and twelve (ten was when I started to feel this way, twelve was when I first really wanted to be dead and thought about killing myself)? And no, please no bright spark go “Aha! Puberty!” because I don’t think that’s it.
So I can see the use of models where it’s “we call this ‘depression’ because it’s majorly depression with some anxiety thrown in, we call that ‘anxiety’ because it’s majorly anxiety with accompanying depression”. That is the problem, really; there are so many things that get dragged into the net of depression – yes, low moods, trouble with sleeping, losing interest in what used to be pleasurable activities, appetite – either lowered or increased, guilt (for some), suicidal thoughts (for others, ranging from “I just want to be dead” to “I am definitely planning to kill myself”), even aches and pains. And these are not unique symptoms, unlike a physical illness where specific rash is “yep, that’s measles not chicken pox”, so they can’t be assigned to only depression or only anxiety.
It helps explain why so many brilliant people searching for The One True Cause Of Depression have come up empty.
I don’t think there is One True Cause. I think it’s very likely there are two major forms of depression: one is the one triggered by stressors (e.g. you are in a bad car crash where you are severely injured and this impacts your quality of life, your job, your personal relationships, being in pain a large amount of the time, etc.) and the one that is biologically based (for want of a better cause) i.e. “well, my boss isn’t yelling at me, I wasn’t in a bad car crash, I’m not homeless and on the streets, why the hell do I want to throw myself off this bridge I cross over every morning?”
On a lighter note, who are these doctors that prescribe Tamiflu and antidepressants the minute you walk in the surgery? Because one of my GPs operated on the attitude that “by the time you show up with the symptoms of the flu, giving you an anti-viral is no use” and I had to nag him into prescribing it for me, and the GP I went to after him was adhering to the new Department of Health policy “as long as you haven’t actually tried to kill yourself, we don’t prescribe anti-depressants anymore, we send you for counselling!” (which is where the CBT came in). Should I move to America? 🙂
Tamiflu is marginally effective at best.
It doesn’t reduce the risk of people with flu being admitted to hospital or developing serious complications.
It slightly increases the risk of adverse effects such as nausea, vomiting, psychiatric and kidney problems.
Slightly reduces the length of symptoms by ~12 hours if taken from the very earliest stage.
Doesn’t really seem worth much.
very meh.
“Who are these doctors that prescribe Tamiflu and antidepressants the minute you walk in the surgery?”
Americans.
Either the medical profession has a much more robust attitude to common illnesses over here (“you are not actually dying? buy some over-the-counter medicine”) or it really does illustrate the difference between health insurance private payer and national health insurance public schemes 🙂
I got Venlafaxine at 150mg/d about five months ago when I visited a new GP for the first time. I’ve been diagnosed with A-typical depression several times in the past, but always under different insurance and at different medical centers. I am not sure the extent to which my medical history is shared across these various people, as they always seem to want me to convince them that I am depressed, but they also always end up giving me some new anti-depressant from the ones I tell them I have tried before. Either I am convincing or they already have my information or they don’t really care. In any case my first time going to see a GP about depression they gave me a script for Lexipro on the spot.
Who are these doctors who will just give you counselling instead of constantly trying to push anti-depressants on you? Should I move to Ireland?
Only if you move to Dublin. Outside the capital there are long waiting lists for counselling and it’s “take what you’re given” (i.e. depending on the particular therapist in your area, they may go for CBT or something else, so not much or indeed any choice).
Dublin gets everything 🙂
We have our own issues here in the USA. Medication is often much easier to get than counseling because generic medication is cheaper than counseling, even factoring in the co-payments or cash payments of going to a psychiatrist. It works out for me because my flavor of brain cooties doesn’t respond well to counseling alone anyway, but those who would prefer counseling are SOL unless they have excellent insurance or lots of money.
That’s fascinating. In fact, I find it so persuasive, I find it hard to imagine *not* thinking something like that.
Although your open questions makes me think a couple of other things.
Firstly, It’s a good sign for the theory if it DOESN’T explain everything. That it helps explain depression and anxiety, but not BPD, suggests it’s an actual theory with useful explanatory power.
(Of course, BPD may be a large amount an underlying cause, and also have self-reinforcing symptoms as well.)
Secondly, there may be extra nodes about the action of biochemical stuff in which are not as visible by looking at someone, but participate in the feedback. The sort of thing sometimes suggested and then withdrawn as one of the candidates for “the” underlying cause. Either acting solely as a driver or influenced by the other symptoms. That means it IS possible to shock someone out of depression with a burst of symptom-treating. And if they were depressed because their life fell apart, but now it’s stable again, that may cure them. But if there’s some biochemical problem as well, it acts like a leaky bucket, and they slowly slip back down into the pit. And to cure them you need a drug which fixes the “leak” AND to reset their current mood with therapy/exercise etc.
That seems to fit more of the evidence, like why sometimes it looks like it has a chemical cause and sometimes it looks like it’s a pattern of symptoms, behaviour and thoughts.
Typo: “the people who write the DSM have really conversations“
I’ve just started reading The Upward Spiral, which argues that depression a pattern of reinforcing behaviors rather than the result of a brain that doesn’t work properly. (Hoping I’ve done the premise justice.)
depression a pattern of reinforcing behaviors rather than the result of a brain that doesn’t work properly
I’d tend to go “yes, but” here.
I think that there are two kinds of depression (just to divide things up crudely); one is triggered by a specific cause like a trauma or stress and the patterns of behaviour that ensue can be a reinforcing loop – that’s the kind of “mild to moderate” depression that CBT can work well for.
Then there’s the “your brain chemistry is fucked” kind of depression, the severe/treatment-resistant kind, that comes out of nowhere with no handy “and the car crash/bank collapse that wiped out your life savings/your wife running off with your twin brother” explanation as to what started the problem and that persists for years even when there is no reason for it to be hanging round. Medication probably is the only help here, CBT or counselling can help to a greater or lesser degree with coping strategies but that won’t shift it on its own (or even make an appreciable dint in the problem).
Thanks for the recommendation. I went out and picked it up immediately.
NDCB approach seems so rigth in retrospect. The only remaining question is “so what?” I have hard time imagining that big pharma endorses the model of a disease without single underlying cause that could be treated with a single agent. So, how this obviously correct model could be used in practice? Any ideas? An app that shows lolcat or advises right medication at the right moment? Facebook newsfeed trained to recognize current user state from word usage and producing sligltly modified contents? A program that optimizes bonuses to achieve better overall happiness of employess weghted by their utility?
A couple of side notes:
1. If I understood it correctly, ketamine effect is due to increased AMPA signaling, which probably translates into increased bottom-up processing. I’m not sure how this could be modeled in network approach by NDCB except as dampening of links between states or maybe adding a lot more noise in transaction between states and some sink-state.
2. I wonder what effects mixing Adderall and Clozaril would produce. Would these two just annihilate each other?
>I have hard time imagining that big pharma endorses the model of a disease without single underlying cause that could be treated with a single agent.
I’m not so sure about that. A symptom based approach seems like an absolute goldmine in a field where you have a large number of co-morbid symptoms that all need to be addressed. Of course, there is the problem that we have a lot of quite reasonable pharmaceutical agents already for things like sleep and inflammation, but still.
Psychiatry has thus far been much more hesitant to embrace this concept of psychopathology compared to Clinical Psych, but they’re starting to pick up on it now.
I’d never heard this model before. Is it well-known and accepted in clinical psych?
We published a review on the literature 2 weeks ago — some of the work has been published in journals such as JAMA psychiatry and PNAS, and Psychological Medicine, Journal of Abnormal Psychology, Journal of Affective Disorders and other have published quite a few papers, too.
At the last clinical conferences such as ABCT, there were always multiple symposia on the network approach (I collected slides from ABCT here). So I’d say that at least in the research world, this approach has been taking off quite well!
The main problem with pharma, as I see it, is that pharma would have little incentive to push this paradigm into clinic. As long as it’s impossible to measure states of patients objectively and reliably, it would be very difficult to organize clinical trials and register drugs that specifically treat e.g. “psychomotor disturbances due to major depression”. It would less risky to develop drug that just treats psychomotor disturbances, regardless of the underlying cause, and then blanket all depressed patients with this drug or leave it at the discretion of psychotherapist.
So, pharma would definitely address as much symptoms as they could, regardless of underlying network dynamics. To use network dynamics would require someone else.
I believe functional medicine tries to approach treatment in a way that would be consistent with this. Functional medicine uses a systems approach to diagnosis and does not just focus on a just few symptoms.
It implies that the FDA’s approach to regulation of prescription drugs is even more broken than we might otherwise believe. If only symptoms exist, not diseases, then telling people they aren’t allowed to take drugs that help with certain symptoms unless they have a certain corresponding disease approved to be treated with that drug looks even more ridiculous.
“The impressive success of ketamine also counts as a point against. NDCB imagine psychiatric disorders like depression as gradually fading out on a symptom-by-symptom basis, eventually reaching a point where enough symptoms are gone that the rest of them aren’t self-reinforcing and just sputter out. This matches the course of eg SSRI treatment, where the medications will gradually improve a few symptoms at at time over the space of a month or so and maybe cause a full remission if you’re lucky. It doesn’t really match ketamine, where every aspect of depression vanishes instantly, then returns after a week or so without treatment. There are a couple of other equally impressive things – staying awake for thirty hours straight, for example, can have an immediate and near-miraculous antidepressant effect, which unfortunately vanishes as soon as you go to sleep. Both of these treatments seem like direct strikes against the One True Cause Of Depression, and both suggest that an underlying tendency toward depression can exist separate from any symptoms (or else why would the depression come back after the effects of the ketamine wore off?)”
I would imagine that handing people a giant wad of cash temporarily cures all symptoms of poverty as well, even though there’s no One True Cause Of Poverty.
Isn’t there one true cause of poverty? Specifically, not having enough money? It sounds like a joke, but that’s exactly the sort of invisible latent variable that depression is being hypothesized not to have.
Or are you saying maybe depression has one true proximate cause being fed into by a number of root causes, like not having enough money is the proximate cause of poverty but there might be root causes like moocher friends or late capitalism or whatever.
Lack of money is a definition, not a cause.
I don’t think you’re following the metaphor. If we look at a cluster of symptoms like frequent worries about money, a deficiency in luxury purchases, and a reluctance to replace worn-out possessions, we might label that cluster as “poverty”. Then, when we discovered that those all stem from a lack of money, we might say “Aha! Poverty is caused by lack of money!” And as we come to understand the money-poverty connection instinctively, we end up identifying poverty as the lack of money itself, rather than a cause. But we’re not there with depression, which is the whole point of the piece, if you follow the metaphor.
For what it’s worth, to say “X is Y by definition” is rarely a useful or insightful contribution. Definitions are just things people use to interpret the world and communicate, they have no fundamental existence.
To clarify this, for myself if nothing else, because i’m not really getting this metaphor.
Suntzu, what you are saying would mean lack of money is influenza right? So poverty is not like depression which is a network of feedback loops, instead it has One True Cause, lack of money.
And Wirehead’s metaphor is supposed to be saying poverty is like depression, so it doesn’t have one true cause, instead it is a network of feedback loops. Maybe things like low(I think it would be low here??) time preference, plasticity, impulse control, etc.
The problem with this metaphor is that in the model of depression the symptoms are the cause, where as the symptoms of poverty are clearly(I think) not the cause of poverty.
There could still be a diffused network of feedback loops that ultimately drive people towards poverty though. Maybe.
Right, but unlike influenza there could be a whole self-reinforcing network prior to the lack of money, all feeding into it, which would explain how there’s one node where you can directly intervene to hit the all the systems, but there’s still a wide array of causes that sometimes reinforce each other and aren’t all always present. I’m not sure if WHWB is hypothesizing something similar for depression, or if WHWB is misunderstanding the metaphor, or if I’m misunderstanding something.
so like
i have no money because:
i like spending money too much
or
i can’t keep track of my money
or
i’m lazy
???
If giving poor people a giant wad of money solved their problems, then you wouldn’t see so many lottery winners crash and burn.
The reality is that lack of money tends to be a symptom of other conditions, rather than an underlying cause. Low IQ correlates with poverty, for instance. So do various other forms of dysfunction.
Poverty itself may not be heritable, but the conditions which correlate with poverty, such as low IQ, certainly are, and others are effectively heritable, such as culture.
I think this reply is mixing up several things, due to differing meanings of “one true cause”.
Like, the question here is, in the causal graph of depression, is there a choke point? Ketamine suggests yes. Here when we talk about “is there one true cause of depression”, we’re not necessarily talking about the things further back that cause that choke point. We’re talking about, is there “one true cause” for the depression symptom cluster. But a lot of things could have causal arrows pointing at that “one true cause”.
When you say, “there’s no one true cause of poverty”, well — “poverty” refers to a lack of money. There’s no mystery there, no hidden phenomenon to look for. “Depression” right now just refers to a symptom cluster, so the question is whether there’s some unified phenomenon behind it; with poverty that question doesn’t even make sense, it already refers to a unified phenomenon. You can say that “there’s no one true cause of poverty”, because lots of things affect the amount of money you have, but that’s a different question, analogous to the many causes that would affect the one-true-cause of depression if it exists.
Or to put it another way, if we had a word “spoverty” that referred to a cluster of different bad things, and then someone realized, hey, whenever a large fraction of these things co-occur, it’s almost always due to a lack of money, then the insight, “Hey, a lack of money is the one true cause of spoverty!” would indeed be a useful insight, even if you didn’t know what caused a lack of money.
(Also, depending on what you consider a “symptom of poverty”, I don’t know that a giant wad of cash necessarily does cure all of them. But the question’s a bit ill-defined, since “poverty”, unlike depression, isn’t defined as a symptom-cluster.)
I mean, “lack of money” isn’t really the sole cause though? It’s “lack of money relative to cost of living” plus, like, having access to certain types of infrastructure and technology at all. Giving a hunter gather in 10,000 B.C. a pocketful of money won’t do jack shit. You could very easily have a symptom cluster model of poverty that consisted of things like “health problems”, “chronic hunger”, “sleeping on a park bench in the middle of winter”, etc etc which to an alien statistician with no understanding of economics or human society would look like a mysterious cluster. Sometimes you would find that curing a lifelong disability cured everything in the “poverty” cluster. Maybe you would find that adding more police officers to the neighborhood helps some people but harms others. You might even find that some people tend to bleed “m factor” no matter how much you try to give them over the long term due to muggings or drug addiction. So I’m not sure this is really all that simple when viewed with fresh eyes.
OK, so I guess what you meant by “poverty” is more like what I meant by “spoverty”? The m-factor is… maybe not a choke-point, exactly, but still something with a lot of direct causal arrows out of it. When everything is going wrong, you can bet on it being involved. Identifying it as money is still big progress.
Sure, obviously the key factor or causal chokepoint can itself has other causes further back, as I said above; it’s not just magically uncaused. But drug addiction can’t bleed an arbitrary amount of money out of a person. You don’t have enough to keep it stabilized, but if you did, you’d see the effects. What you have is A -> B -> other effects; you could say that “the real cause is A, not B”, and in many cases the best solution will be to fix A, so that it doesn’t keep exerting its downstream influence; but in other cases it may be easier instead to hold B in place directly, breaking the A->B link. (Insert medical example here.)
OTOH, if your key factor is involved in feedback loops with the symptoms — which in the spoverty case it certainly would appear to be — then maybe calling it “the one true cause” is a bit misleading. It still might be true that holding it fixed with all your might could solve the other problems, but its position in the network is less privileged. Focusing on it alone makes less sense.
Poverty can be considered as analogous to a single node in the network more easily than it can be considered symptom cluster. A high course-load at uni, shift work, anxiety problems, or jetlag can all cause insufficient sleep, and Ambien can cure insufficient sleep in most of those cases. Both poverty and insufficient sleep are affected by many things, but have a definition aside from that. Depression is practically defined by a multitude of symptoms.
You’re careful to say “every aspect of depression” for ketamine, but I wonder if people have actually studied it with the graph of self-reinforcing symptoms in mind, and what they would find if they did.
Yeah, I should admit I’m basing that off of vague impressions rather than any good study.
This made me think of the Maudsey (sp?) treatment for anorexia, which is simply make the patient eat and eat until they are comfortably within proper weight, then make sure they maintain the weight. It’s the one treatment that’s been shown to work in children (obviously it’s harder to implement in legal adults), one of my cousins underwent it, successfully. Her father said the therapist just ignored all the psychological symptoms, saying “if they don’t come right of themselves as she regains the weight, we’ll treat them later.” And the psychological symptoms came right.
I’ve read about it, and the developers are apparently formally agnostic about what starts anorexia, but they hypothesise that it starts with a loss in body weight, be that through deliberate dieting or ill-health due to a virus or whatever, and then in some people the weight loss sends their brain on a downward spiral. The limitation of the treatment, apart from legal issues with adults, is that if a weight loss reoccurs, so does the anorexia.
Two points:
1) Scott, re: Viibryd. At some point in the past you expressed a sentiment that you did not know anyone who had ever decreased depression on Viibryd. Expressing it as, IIRC, “Seriously, fuck Viibryd”. Anecdotally, I have good effects from 5 mg. My daughter takes 40 mg, along with a bunch of other things as well. Again, just anecdotal, but, I figured it might be mildly useful.
2) My mood really managed to rebound to “normal” levels (still depressed, but a much milder form) when I finally took my wife’s repeated advice and had a sleep study done. Being treated for age-related obstructive sleep apnea has been a uniformly positive experience that has done wonders for my deep depression.
Thanks for the Viibryd tip. I have a patient I need to use one of the newer agents on for various reasons, and it’s good to know that someone’s found success with them.
@Scott Alexander:
I should probably further point out that, I have an ADHD diagnosis and I also am on Adderall XR. As is my daughter. She also has a bipolar diagnosis and is on Lamictal and Abilify.
As support for the multiple points of interacting feedback hypothesis, my ADHD diagnosis, Apnea diagnosis and a low testosterone diagnosis all happened around the same time (within months of each other). Apnea can actually lead to low-testosterone, so that’s a feedback loop within a feedback loop.
Sorry to drag down the tone of this excellent post, but I honestly cannot read that name – Viibryd – without thinking it’s one of the new generation sex toys (you know, for empowered liberated women), one of the ones all ergonomic curves and not looking anything like traditional vibrators – er, not that I’d know anything about that 🙂
To me it looks like some Welsh hamlet.
As thoughtcrimes go, yours has the advantage at least of being entertaining.
Now if you’ll just put on these handcuffs…
(that said, one could plausibly argue that the resemblance is either intentional or a side benefit – “sex sells” after all)
I haven’t read the paper, but you seem to go back and forth between two models that you attribute to NDCB. The weak hypothesis is “What if it’s symptoms all the way down?” The strong hypothesis is that it is self-reinforcing patterns of symptoms.
A lot of what you said confused me because I thought that you were talking about the weak claim, but I now think you were talking about the strong one. A lot of physical conditions are probably just clusters of symptoms. You even mentioned one — inflammation. But it probably isn’t a self-reinforcing pattern.
If different people have different edge strengths, you’d get variation in the clusters – and it doesn’t take too much messing with the edge strengths to change the clustering pretty heavily.
Also, depending on the edge strengths, different things might be the centre of the cluster for different people. And I think hitting the centre of the cluster hard is more effective than hitting all vertices simultaneously (even before you account for drug interactions messing things up). This would explain why different antidepressants are better for different people.
(Also, finally a post about spectral graph theory. Hooray for my field!)
I think that “blasting all symptoms at once” could partially not work because of drug interactions and so on. Like, if you’re using marijuana to increase appetite and stimulants for motivation then the benefits of each of those will be reduced, since marijuana can reduce motivation and stimulants can decrease appetite.
Which suggests that the limited side-effects from anti-depressants is actually important regarding their broad effectiveness, I think. Stimulants are highly effective at treating some symptoms, and worsen others, so for many people it won’t actually be effective overall, or it might be counterproductive, whereas for some people the effect the “not having energy” node was having makes the tradeoff worthwhile.
This was my thought as well. Based on my observations of people who “treat” themselves with marijuana, it seems like the laziness and detachment that marijuana promotes would be difficult to simply cancel out with, say, Adderal, and you’d end up with a jittery affectless drone who still seems and is depressed.
Yes, okay, fine, that was just an example. We can use Remeron for appetite if you want…hey, wait!
Scott, give Periactin a try for appetite instead of Remeron. Periactin doesn’t have such a whopping H2 antagonism as Remeron and it doesn’t cause so much hangover and daytime drowsiness. Shorter half-life also helps.
I did look at the suggested list for for treating depression and immediately think “Yes, and then you die.”
At a certain point, it actually seems plausible that treating all the symptoms of depression would either cure it (and you could quit taking drugs) or suppress it (and you’d continue indefinitely). The problem there is just that once you’re hopped up on that frankly spectacular list of chemicals, you’re likely to be feeling absolutely terrible for a lot of reasons unrelated to the original depression. Treating fewer symptoms has fewer side effects (we can regulate sleep pretty well) but also achieves less.
If psychiatric disorders are ultimately more correctly modeled as something like NDCB, what does that say about the value of the DSM? Is it the record of a valiant 50 year attempt that’s ultimately worthless?
Ever since I learned that the NIMH is “re-orienting away” from funding studies based on the DSM I’ve been skeptical of it. But there was nothing really to take its place, that I knew of. This is an interesting approach.
Not really. It would still have value the same way that naturalists’ observation about different species had value before we understood genetics and evolution. It’s true that certain collections of symptoms tend to go together, and the DSM is a good record of that.
If you look at the paper itself, it actually uses DSM symptoms as part of its networking process.
Research Domain Criteria (RDoC), which was mentioned in that NIMH post as what they’re orienting to, seems like a really useful tool for research and I can’t help but wonder if it’ll wind up in the clinic as well. It gets at a lot of the things Scott brings up in this post about uncovering the underlying biology and looking at the symptoms dimensionaly etc. Because if we assume that the symptoms are ultimately a product of the neurobiology, then clearly identifying those symptoms can shine a light on what’s actually changed, and that’s usually a good first step to fixing something.
A good example of RDoC in practice is this study by Clementz from April. Press release is here. They took hundreds of psychotic individuals diagnosed with Schizophrenia, Schizoaffective or Psychotic Bipolar, hundreds of their relatives, and still hundreds more healthy controls (it was a giant god damn study) and then gave them a battery of psychometric tests and brainscans and wound up separating them into three entirely new groups based on what they call Cognitive Control and Reactivity. Each of the groups, what they call biotypes, had members from all three of the original groups, illustrated here. The big idea being that with this separation, they’ll be able to better target therapies and interventions. Don’t know how well they’ve followed up with that though.
tl/dr I think RDoC is great for scientists, I hope it’ll be good for patients too.