There’s been recent controversy about the use of face masks for protection against coronavirus. Mainstream sources, including the CDC and most of the media say masks are likely useless and not recommended. They’ve recently been challenged, for example by Professor Zeynep Tufekci in the New York Times and by Jim and Elizabeth on Less Wrong. There was also some debate in the comment section here last week, so I promised I’d look into it in more depth.
As far as I can tell, both sides agree on some points.
They agree that N95 respirators, when properly used by trained professionals, help prevent the wearer from getting infected.
They agree that surgical masks help prevent sick people from infecting others. Since many sick people don’t know they are sick, in an ideal world with unlimited mask supplies everyone would wear surgical masks just to prevent themselves from spreading disease.
They also agree that there’s currently a shortage of both surgical masks and respirators, so for altruistic reasons people should avoid hoarding them and give healthcare workers first dibs.
But they disagree on whether surgical masks alone help prevent the wearer from becoming infected, which will be the focus of the rest of this piece.
1. What are the theoretical reasons why surgical masks might or might not work?
Epidemiologists used to sort disease transmission into three categories: contact, droplet, and airborne. Contact means you only get a disease by touching a victim. This could be literally touching them, or a euphemism for very explicit contact like kissing or sex. Droplet means you get a disease when a victim expels disease-laden particles into your face, usually through coughing, sneezing, or talking. Airborne means you get a disease because it floats in the air and you breathe it in. Transmission via “fomites”, objects like doorknobs and tables that a victim has touched and left their germs on, is a bonus transmission route that can accompany any of these other methods.
More recently, scientists have realized that droplet and airborne transmission exist along more of a spectrum. Droplets can stay in the air for more or less time, and spread through more or less volume of space before settling on the ground. The term for this new droplet-airborne spectrum idea is “aerosol transmission”. Diseases with aerosol transmission may be spread primarily through droplets, but can get inhaled along with the air too. This concept is controversial, with different authorities having different opinions over which viruses can be aerosolized. It looks like most people now believe aerosol transmission is real and applicable to conditions like influenza, SARS, and coronavirus.
Surgical masks are loose pieces of fabric placed in front of the mouth and nose. They offer very good protection against outgoing droplets (eg if you sneeze, you won’t infect other people), and offer some protection against incoming droplets (eg if someone else sneezes, it doesn’t go straight into your nose). They’re not airtight, so they offer no protection against airborne disease or the airborne component of aerosol diseases.
Respirators are tight pieces of fabric that form a seal around your mouth and nose. They have various “ratings”; N95 is the most common, and I’ll be using “N95 respirator” and “respirator” interchangably through most of this post even though that’s not quite correct. When used correctly, they theoretically offer protection against incoming and outgoing droplet and airborne diseases; since aerosol diseases are a combination of these, they offer generalized protection against those too. Hospitals hate the new “aerosol transmission” idea, because it means they probably have to switch from easy/cheap/comfortable surgical masks to hard/expensive/uncomfortable respirators for a lot more diseases.
Theory alone tells us surgical masks should not provide complete protection. Coronavirus has aerosol transmission, so it is partly airborne. Since surgical masks cannot prevent inhalation of airborne particles, they shouldn’t offer 100% safety against coronavirus. But theory doesn’t tell us whether they might not offer 99% safety against coronavirus, and that would still be pretty good.
2. Are people who wear surgical masks less likely to get infected during epidemics?
It’s unethical to randomize people to wear vs. not-wear masks during a pandemic, so nobody has done this. Instead we have case-control studies. After the pandemic is over, scientists look at the health care workers who did vs. didn’t get infected, and see whether the infected people were less likely to wear masks. If so, that suggests maybe the masks helped.
This is an especially bad study design, for two reasons. First, it usually suffers recall bias – if someone wore a mask inconsistently, then they’re more likely to summarize this as “didn’t wear masks” if they got infected, and more likely to summarize it as “did wear masks” if they stayed safe. Second, probably some nurses are responsible and do everything right, and other nurses are irresponsible and do everything wrong, and that means that if anything at all helps (eg washing your hands), then it will look like masks working, since the nurses who washed their hands are more likely to have worn masks. Still, these studies are the best we can do.
Gralton & McLaws, 2010 reviews several studies of this type, mostly from the SARS epidemic of the early 2000s. A few are underpowered and find that neither surgical masks nor respirators prevent infection (probably not true). A few others show respirators prevent infection, but do not investigate surgical masks (probably right, but useless for our purposes). Two seem relevant to the question of whether surgical masks work:
Rapid awareness and transmission of SARS in Hanoi French Hospital, Vietnam was conducted in a poor hospital that only had surgical masks, not respirators. In the latter stages of the epidemic, 4 workers got sick and 26 stayed healthy. It found that 3 of the 4 sick workers hadn’t been wearing masks, but only 1 of the 26 healthy workers hadn’t. This is a pretty dramatic result – subject to the above confounders, of course.
Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of SARS is larger and more prestigious, and looked at a cluster of five hospitals. Staff in these hospitals used a variety of mask types, including jury-rigged paper masks that no serious authority expects to work, surgical masks, and N95 respirators. It found that 7% of paper-mask-wearers got infected, compared to 0% of surgical-mask and respirator wearers. This seems to suggest that surgical masks are pretty good.
The meta-analysis itself avoided drawing any conclusions at all, and would not even admit that N95 respirators worked. It just said that more research was needed. Still, the two studies at least give us a little bit of evidence in surgical masks’ favor.
How concerned should we be that these studies looked at health care workers specifically? On the one hand, health care workers are ordinary humans, so what works for them should work for anyone else. On the other, health care workers may have more practice using these masks, or may face different kinds of situations than other people. Unlike respirators, surgical masks don’t seem particularly hard to use, so I’m not sure health care workers’ training really gives them an advantage here. Overall I think this provides some evidence that surgical masks are helpful.
I was able to find one study like this outside of the health care setting. Some people with swine flu travelled on a plane from New York to China, and many fellow passengers got infected. Some researchers looked at whether passengers who wore masks throughout the flight stayed healthier. The answer was very much yes. They were able to track down 9 people who got sick on the flight and 32 who didn’t. 0% of the sick passengers wore masks, compared to 47% of the healthy passengers. Another way to look at that is that 0% of mask-wearers got sick, but 35% of non-wearers did. This was a significant difference, and of obvious applicability to the current question.
3. Do surgical masks underperform respirators in randomized trials?
Usually it would be unethical to randomize health care workers to no protection, so several studies randomize them to face masks vs. respirators. But a few others were done in foreign hospitals where lack of protection was the norm, and these studies did include a no-protection control group.
MacIntyre & Chugtai 2015, Facemasks For The Prevention Of Infection In Healthcare And Community Settings, reviews four of these. Two of the four are unable to find any benefit of either masks or respirators. The third finds a benefit of respirators, but only if nobody tested the respirators to see if they fit, which doesn’t make sense and suggests it’s probably an artifact. The fourth finds a benefit of respirators, but not masks. It seems unlikely that respirators don’t help, so this suggests all these studies were underpowered. If we throw good statistical practice to the winds and just look at the trends, they look like this:
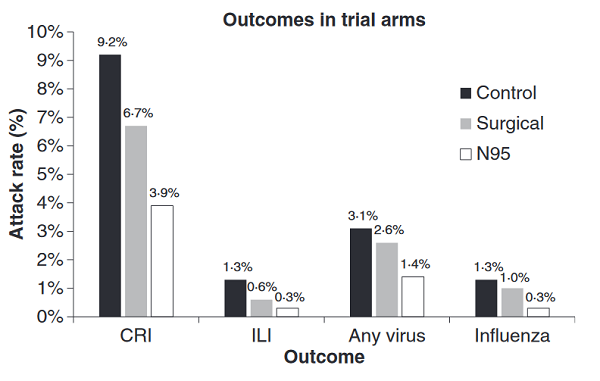
In other words, respirators are better than masks are better than nothing. It would be wrong to genuinely conclude this, because it’s not statistically significant. But it would also be wrong to conclude the studies show masks don’t work, because they mostly show respirators don’t work, and we (hopefully) know they do.
Overall these studies don’t seem very helpful and I’m reluctant to conclude anything from them. In section 6, I’ll talk more about why studies may not have shown any advantage for respirators.
4. Do surgical masks prevent ordinary people from getting infected outside the healthcare setting?
The same review lists nine randomized trials with a different design: when the doctor diagnoses you with flu, she either asks everyone in your family to wear masks (experimental group), or doesn’t do that (control group), and then checks how many family members in each group got the flu.
How did these go? That depends whether you use intention-to-treat or per-protocol analysis. Intention-to-treat means that you just compare number of infections in the assigned-to-wear-masks group vs. the control group. Per-protocol means that you only count someone in the study if they actually followed directions. So if someone in the assigned-to-wear mask group didn’t wear their mask, you remove them from the study; if someone in the control group went rogue and did wear a mask, you remove them too.
Both of these methods have their pros and cons. Per protocol is good because if you’re trying to determine the effect of wearing a mask, you would really prefer to only be looking at subjects who actually wore a mask. But it has a problem: adherence to protocol is nonrandom. The people who follow your instructions diligently are selected for being diligent people. Maybe they also diligently wash their hands, and diligently practice social distancing. So once you go per protocol, you’re no longer a perfect randomized controlled trial. Only intention-to-treat analyses carry the full weight of a gold standard RCT.
According to intention-to-treat, the studies unanimously found masks to be useless. But there were a lot of signs that intention-to-treat wasn’t the right choice here. Only about a fifth of people who were asked to wear masks did so with any level of consistency. The rest wore the mask for a few hours and then get bored and took it off. Honestly, it’s hard to blame them; these studies asked a lot from families. If a husband has flu, and sleeps in the same bed as his wife, are they both wearing masks all night?
Of the three studies that added per-protocol analyses, all three found masks to be useful (1, 2, 3) . Does this prove masks work? Not 100%; per-protocol analyses are inherently confounded. But it sure is suggestive.
The review author summarizes:
The routine use of facemasks is not recommended by WHO, the CDC, or the ECDC in the community setting. However, the use of facemasks is recommended in crowded settings (such as public transport) and for those at high risk (older people, pregnant women, and those with a medical condition) during an outbreak or pandemic. A modelling study suggests that the use of face-masks in the community may help delay and contain a pandemic, although efficacy estimates were not based on RCT data. Community masks were protective during the SARS outbreaks, and about 76% of the population used a facemask in Hong Kong.
There is evidence that masks have efficacy in the community setting, subject to compliance [13] and early use [12, 18, 19]. It has been shown that compliance in the household setting decreases with each day of mask use, however, which makes long term use over weeks or months a challenge […]
Community RCTs suggest that facemasks provide protection against infection in various community settings, subject to compliance and early use. For health-care workers, the evidence suggests that respirators offer superior protection to facemasks.
Parts of this summary are infuriating. If the big organizations recommend that especially vulnerable groups wear masks, aren’t they admitting masks work? But if they’re admitting masks work, why don’t they recommend them for ordinary people?
It looks like they’re saying masks work a little, they’re too annoying for it to be worth it for normal people, but they might be worth it for the especially vulnerable. But then why don’t they just say masks work, and let each person decide how much annoyance is worthwhile? I’m not sure. But it looks like the author basically ends up in favor of community use of surgical masks in a pandemic, mostly on the basis of per-protocol analyses of community RCTs.
5. How do surgical masks and respirators compare in hokey lab studies?
Our source here is Smith et al 2016, Effectiveness Of N95 Respirators Versus Surgical Masks In Protecting Health Care Workers From Acute Respiratory Infection: A Systematic Review And Meta-Analysis. They review some of the same studies we looked at earlier, but then investigate 23 “surrogate exposure studies”, ie throwing virus-shaped particles at different masks in a lab and seeing if they got through. You can find the results of each in their appendix. Typically, about 1 – 5% of particles make it through the respirator, and 10 – 50% make it through the surgical mask. They summarize this as:
In general, compared with surgical masks, N95 respirators showed less filter penetration, less face-seal leakage and less total inward leakage under the laboratory experimental conditions described.
I think in general the fewer virus particles get through your mask, the better, so I think this endorses surgical masks as better than nothing, since their failure rate was less than 100%.
Booth et al, 2013 examines surgical masks themselves more closely. They hook a surgical mask up to “a breathing simulator” and then squirt real influenza virus at it, finding that:
Live influenza virus was measurable from the air behind all surgical masks tested. The data indicate that a surgical mask will reduce exposure to aerosolised infectious influenza virus; reductions ranged from 1.1- to 55-fold (average 6-fold), depending on the design of the mask…the results demonstrated limitations of surgical masks in this context, although they are to some extent protective.
The paper doesn’t discuss how particle number maps to infection risk. Does letting a single influenza virus through mean you will get infected? If so, any reduction short of 100% is useless. I have a vague sense that this isn’t true; your immune system can fight off most viruses, and the fewer you get, the better the chance it will win. Also, even respirators don’t claim to reduce particle load by more than 99% or so, and those work, so it can’t be that literally a single virus will get you. Overall I think modest reductions in particle number are still pretty good, but I don’t have a study that proves it.
6. Is it true that the public won’t be able to use N95 respirators correctly?
Yes.
I remember my respirator training, the last time I worked in a hospital. They gave the standard two minute explanation, made you put the respirator on, and then made you go underneath a hood where they squirted some aerosolized sugar solution. If you could smell the sugar, your respirator was leaky and you failed. I tried so hard and I failed so many times. It was embarrassing and I hated it.
I’m naturally clumsy and always bad at that kind of thing. Some people were able to listen to the two minute explanation and then pass right away. Those kinds of people could probably also listen to a two minute YouTube explanation and be fine. So I don’t want to claim it’s impossible or requires lots of specialized background knowledge. It’s just a slightly difficult physical skill you have to get right.
Bunyan et al, 2013, Respiratory And Facial Protection: A Critical Review Of Recent Literature, discusses this in more depth. They review some of the same studies we reviewed earlier, showing no benefit of N95 respirators over surgical masks for health care workers in most situations. This doesn’t make much theoretical sense – the respirators should win hands down.
The most likely explanation is: doctors aren’t much better at using respirators than anyone else. In a California study of tuberculosis precautions, 65% of health care workers used their respirators incorrectly. That’s little better than the general public, who have a 76% failure rate. Bunyan et al note:
The fitting of N95 respirators has been the subject of many publications. The effective functioning of N95 respirators requires a seal between the mask and the face of the wearer. Variation in face size and shape and different respirator designs mean that a proper fit is only possible in a minority of health care workers for any particular mask. Winter et al. reported that, for any one of three widely used respirators, a satisfactory fit could be achieved by fewer than half of the healthcare workers tested, and for 28% of the participants none of the masks gave a satisfactory fit.
Fit-testing is a laborious task, taking around 30 min to do properly, and comprises qualitative fit-testing (testing whether the respirator-wearing healthcare worker can taste an intensely bitter or sweet substance sprayed into the ambient air around the outside of the mask) or quantitative fit testing (measuring the ratio of particles in the air inside and outside the breathing zone when wearing the respirator). Attempts have been made to circumvent the requirement for fit testing, and it has been suggested that self-testing for a seal by the respirator wearer (see http://youtu.be/pGXiUyAoEd8a for a video demonstration) is a sufficient substitute for fit-testing. However, self-checking for a seal has been demonstrated to be a highly unreliable technique in two separate studies so that full fit-testing remains a necessary preliminary requirement before respirators can be used in the healthcare setting.
Operationally, this presents significant challenges to organizations with many healthcare workers who require fit-testing. Chakladar et al. pointed out that, in addition to the routine need for repeat testing over time to ensure that changes in weight or facial hair have not compromised a good fit, movements of healthcare workers between organizations using different makes of respirators would necessitate additional repeat fit-testing. Fit-testing is likely to remain problematic to health-care organizations for the foreseeable future. In addition to the requirement for fit-testing, ‘fit-checking’ is also required each time the respirator is donned to ensure there are no air leaks.
Is a poorly-fitting N95 respirator better than nothing? The reviewed studies suggest that at that point it’s just a very fancy and expensive surgical mask.
7. Were the CDC recommendations intentionally deceptive?
No, and I owe them an apology here.
I think the evidence above suggests masks can be helpful. Masked health care workers were less likely to catch disease than unmasked ones. Masked travelers on planes were less likely to catch disease than unmasked ones. In per protocol analysis, masked family members are less likely to catch disease from an index patient than unmasked ones. Laboratory studies confirm that masks block most particles. All of this accords with a common-sense understanding of droplet and aerosol transmission of disease.
None of these, except maybe the plane study, tell us exactly what we want to know. The SARS studies were all done in a health care setting, so they don’t prove that regular people can benefit from masks. But health care workers are closely related to homo sapiens and ought to have similar anatomy and physiology. Surgical masks aren’t as complicated as respirators and we can assume most people get them right. And although health care workers are in unusually high-risk situations, that should just affect the magnitude of the benefit, not the sign; obviously the level of risk ordinary people encounter is sometimes relevant, considering they do often catch pandemic diseases. So our default assumption should be that these studies carry over, not that they don’t.
Likewise, most of the community studies were done on family members. Most guidelines already say to mask up if you have a sick family member, so talking about subways and crowds requires a little bit of extrapolation. But again, being in a family is just one form of close contact. It would take bizarre convolutions to even imagine a theory where you can catch diseases from your family members but not from people you sit next to on a train. Our default assumption should be in favor of these results generalizing, not against them.
But the CDC has recommended against mask use. I hypothesized that the CDC was intentionally lying to us, trying to trick us into not buying masks so there would be enough for health care workers.
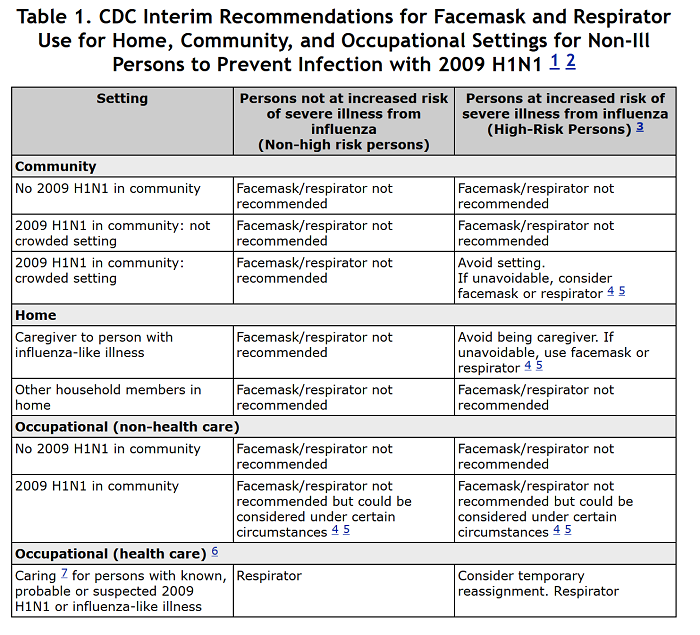
But that can’t be true, because the CDC and other experts came up with their no-masks policy years ago, long before there was any supply shortage. For example, during the 2009 swine flu pandemic, their website offered the following table:
And during the 2015 MERS epidemic, NPR said South Koreans were wrong to wear masks:
Masks can be helpful for protecting health workers from a variety of infectious diseases, including MERS…
But either type of mask is less likely to do much good for the average person on the street…Wearing a mask might make people feel better. After all, MERS has killed about a third of the people known to be infected.
But there are no good studies looking at how well these masks prevent MERS transmission out in the community, says Geeta Sood, an infectious disease specialist at Johns Hopkins University. “On the street or the subway, for MERS specifically, they’re probably not effective,” she says. One problem is that the masks are loose fitting, and a lot of tiny airborne particles can get in around the sides of the masks.
So if studies generally suggest masks are effective, and the CDC wasn’t deliberately lying to us, why are they recommending against mask use?
I’m not sure. I haven’t been able to track down any documents where they discuss the reasons behind their policies. It’s possible they found different studies than I did, or interpreted the studies differently, or have some other superior knowledge.
But I think that more likely, they’re trying to do something different with medical communication. Consider legal communication. If a court declares a suspect is “not guilty”, that could mean that he is actually not guilty of the crime. Or it could mean that he did it but they can’t prove it. Or it could mean that he did it, they can prove it, but the police officer who found the proof didn’t have a warrant at the time so they had to throw it out. A legal communication like “this man is not guilty” is intended not just to convey information, but to formally reflect the output of a sacrosanct process.
Medicine has been traumatized by its century-long war with quackery, and ended up with its jargon also formally reflecting the output of a sancrosanct process. Remember, there are dozens of studies supposedly showing homeopathy works, not to mention even more studies proving telepathy exists. At some point you have to redesign all your institutions to operate in an environment of epistemic learned helplessness, and the result is very high standards of proof.
Masks haven’t quite reached these standards. The case-control trials look good, and the per-protocol RCTs look good, but there aren’t really the large-scale intention-to-treat RCTs that would be absolutely perfect. Even if these studies work, they only prove things about the health care setting and the family setting, not “the community setting” in general. So masks haven’t been proven to work beyond a reasonable doubt. Just like the legal term for “not proven guilty beyond a reasonable doubt” is “not guilty”, the medical communication term for “not proven effective beyond a reasonable doubt” is “not effective”. This already muddled communication gets even worse because doctors are constitutionally incapable of distinguishing “no evidence for” from “there is evidence against” – I have no explanation for this one.
There’s an even more complicated language-use issue. The CDC may be thinking of its recommendations not just as conveying an opinion but as taking an action – performing the medical intervention of recommending people wear masks. All of those RCTs listed above show that the medical intervention of recommending people wear masks is ineffective. Sure, that’s because people don’t listen. But the CDC doesn’t care about that. They’ve proven that giving the advice won’t help, why are you still asking them to give the advice?
I’m not sure this is really the CDC’s reasoning. It seems pretty weird from the point of view of an organization trying to manage a real-world pandemic with people dying if they get it wrong. But I’m having trouble figuring out other possibilities that make sense.
8. So should you wear a mask?
Please don’t buy up masks while there is a shortage and healthcare workers don’t have enough.
If the shortage ends, and wearing a mask is cost-free, I agree with the guidelines from China, Hong Kong, and Japan – consider wearing a mask in high-risk situations like subways or crowded buildings. Wearing masks will not make you invincible, and if you risk compensate even a little it might do more harm than good. Realistically you should be avoiding high-risk situations like subways and crowded buildings as much as you possibly can. But if you have to go in them, yes, most likely a mask will help.
In low-risk situations, like being at home or taking a walk, I mean sure, a mask might make you 0.0001% (or whatever) less likely to get infected. If that’s worth it to you, consider the possibility that you might be freaking out a little too much about this whole pandemic thing. If it’s still worth it, go for it.
You are unlikely to be able to figure out how to use an N95 respirator correctly. I’m not saying it’s impossible, if you try really hard, but assume you’re going to fail unless you have some reason to think otherwise. The most likely outcome is that you have an overpriced surgical mask that might make you incorrectly risk-compensate.
If you are a surgeon performing surgery, bad news. It turns out surgical masks are not very useful for you (1, 2)! You should avoid buying them, since doing so may deplete the number available for people who want to wear them on the subway.

















In the event that surgical masks become widely and cheaply available to the public, should we encourage everyone to wear one when in public, to reduce asymptomatic infected people infecting others?
In the mean time, should we be creating cloth masks for this purpose?
After reading this post, I find the “cloth mask” question pretty pressing. Do the data presented here apply to any piece of fabric placed over the nose and mouth? Or do surgical masks have some special properties that e.g. a scarf or bandana wouldn’t have?
Moreover, how much of the value is lost by re-using a mask? My guess is that it would still stop you from transmitting to others, but wouldn’t provide any protection to you because the virus can easily transmit to the mouth-facing side when taken on and off. Is that right, or am I fundamentally misunderstanding?
This post doesn’t do as good a job as usual at explaining things or looking at the evidence, and you shouldn’t think surgical masks are the same as cloth masks because of it.
Surgical masks are mostly made from paper (or other non-woven material). Cloth masks work worse than them according to the studies I’ve found.
https://academic.oup.com/cid/article/65/11/1934/4068747
https://link.springer.com/article/10.1186/1756-0500-6-216
It’s unclear, but one important reason that homemade cloth masks are a plausibly good idea is that wearers 1) won’t touch their face quite as much, and may remember to wash their hands better, 2) indicate that people in public are taking the risk seriously, and 3) don’t reduce the supply available to doctors and hospitals in the short term.
Also, to the extent the spread is because I cough and a biggish droplet lands on your mouth, a bandana will help with that. And big particles that have to make an extra right-angle turn to get into your lungs may also just not make it in. That’s not going to do much for the really tiny airborne dried-out droplets, but think of the times you’ve been close to someone when they sneeze, cough, or speak, and felt a droplet touch your skin–that’s happened to me, and if they’re infected and shedding virus, you’ve not got some infectious virus on you waiting to be rubbed into your eye or something.
The droplet that would have entered your mouth instead lands on the fabric, where the water evaporates, leaving airborne virus that you inhale.
N95 masks work in part because the holes in the mask/filter media are smaller than some dimensions of the virus. Fabric has holes on the micron scale.
@deciusbrutus:
Our instincts are very different here. My instinct, based on experience using often ill-fitting masks for paint, dust, smoke and solvent protection, is that all masks provide at least some benefit, and that any amount of direct exposure that can be prevented is a good thing. Yes, some of the virus will eventually be inhaled, but don’t you agree that the dosage of active virus will be less than if there was no mask? Some will remain dried on the mask, some (half?) will be blown away on an exhale, and some of what is inhaled will have been deactivated by the drying.
We lack exact numbers, but I’d hope you’d agree that the mask provides some reduction in exposure? Is it that you believe that infection is almost sure to occur over a small threshold, and thus this reduction provides no added protection? That the reduction can only be such a small amount that degree of protection should be ignored? Or something else? It feels like you are (correctly) pointing out that the protection is not perfect, and then jumping to the conclusion that the degree of protection that is provided is thus irrelevant.
decibrutus:
If that mechanism works, why does anyone ever wear a surgical mask?
@deciusbrutus:
CoV19 is very likely not airborne, probably due to being inactivated when drying. So for anthrax your comment would be correct, for CoV19 it is most probably not.
Some countries like the Czech republic and maybe the CDC do recommend cloth face covers as an alternative to masks. As a general question, this is probably very hard to answer, because there are too many variables. One layer of chiffon net is probably not going to do anything. On the other end of the spectrum, with tightly woven cloth and relevant expertise you could probably create a pretty good filter mask.
How you wear the mask is also really important. If your scarf keeps slipping of your face, or makes you itchy, you may well end up touching your face much more than you otherwise would. That’s probably a net negative.
Homemade fabric masks range from ~half as effective as surgical masks to ~about as effective as surgical masks in terms of raw filtration power, but have two downsides:
1. Universally, they don’t fit as well, leading to leakage around the edges. (That part of the study had volunteers make their own from a pattern.)
2. The ones that filter as well as surgical masks are much more difficult to breathe through, and the ones that are as easy to breathe through don’t filter as well.
https://www.researchgate.net/publication/258525804_Testing_the_Efficacy_of_Homemade_Masks_Would_They_Protect_in_an_Influenza_Pandemic#pf7
Since my wife is a hospital medicine doc at a hospital that is short of supplies, a friend and I have been working on masks. She has made both the rectangular pleated and the ‘Fu Face Mask’ types.
1. At least for the mid-weight cotton fabric we have used, an easy way to test is to wet the fabric thoroughly; it is then nearly impossible to breathe through, and leaks are easily detectable. (The fabric is breathable again as soon as it dries.)
2. The primary failure mode of both mask designs seems to be leakage on either side of the nose.
3. It isn’t hard to fashion a nose bridge to shape the fabric to the skin. License plates are made of a soft aluminum alloy and about the right thickness. They can be cut with a good pair of scissors.
4. I formed the metal with my fingers, then attached with VHB outdoor-rated tape, but it might be more durable to sew them on to the outer layer of fabric with embroidery thread (best to let the inner layer free, as it sort of sucks in against the face and improves the seal on inhalation).
This seems kind of important to leverage the efforts of many crafty types who are making masks; I’m not a social media person so not sure how to better promote.
Hi Quercus,
I really want to get involved in this. I’m working on a website to bring together some patterns and instructions (mainly to make it easy to download and print), what we know about which design and materials are effective, how to find places to donate them to, etc. Basically trying to make this info available in one place so people don’t have to search for it.
I sew, but I live on a boat, and I don’t have an iron or any idea how to set one up safely. I plan to make a few masks to learn how, and then focus on writing up what I’ve learned and spreading it around. I’m not really a social media person either, but I know how to set up a website and could probably figure out how to make infographics that are easily shared and stuff. (I’m a programmer, and past hobbies have involved WordPress and photoshop)
It would be really helpful to be able to consult someone who’s producing lots of masks and “gets” the rationalist/ea/whatever approach to things. If you’re willing to chat about it, would you mind sending me an email so we can connect? My email is my username, at Gmail.
Vacuum cleaner bags have tiny pores (better than other materials except surgical masks, but not enough for virus particles).
You can use the existing seams to create a shape with a large surface to breathe through (less pressure and less airflow per area! => easier breathing, lower pressure differential between the mask area and gaps around it!).
If the material has a minimal stiffness, you might end up with something in the shape of a beak or snout (and look like the plague doctors in medieval woodcuts 🙂 ).
ETA: Don’t make big volumes or the wearer will only re-inhale their own exhalated volume… Evolution a work 🙂
ETA2: One bag for in- and one for exhalation, a valve, and something like a snorkel’s mouthpiece? 🙂
Early Modern woodcuts. There are such things as Late Medieval woodcuts, but there are no beaky plague doctors in them, that was a later era.
Thanks!
That’s what I really love about SSC — expose some dumbness and be not allowed to go uncorrected!
I think this is exactly the only right and relevant question at this time. The remainder of the discussion is just noise. Everyone agrees “that surgical masks help prevent sick people from infecting others”. Whether they also protect you is irrelevant: you have your priorities wrong if that’s what you are arguing about (sorry Scott, from a technical point of view this is again a very interesting article, but it’s just not important at the moment and any subsequent discussion about its contents is currently just noise)
> Whether they also protect you is irrelevant
huh. Irrelevant to what?
I personally would like to know, for myself and for others, whether they do protect you. And I’m pretty sure they do. A bit. But I’m happy to get some measure of confirmation.
Sorry, “Confusion”, if my concerns for the protection of myself and those close to me are “just not important”. No, actually: not sorry.
It’s irrelevant whether they protect you, because if we all agree they protect others against you, then everyone should already be wearing them. Arguing about whether they also additionally protect you is a distraction. If you worry about your health, you should be focussing on getting everyone else to wear a face mask. Listening to your selfish impulses and not taking the outside view leads to the wrong priorities that do not lead to an optimal outcome for you.
That is not correct. The result of my listening to my selfish impulses and acting for my own self interest is the optimal outcome for me, although not necessarily for the world.
If advising other people to wear face masks reduces the risk to me by enough to be worth the effort, then my selfish impulses will lead me to do it. My guess is that it doesn’t — the number of people I would persuade, if any, would be such a tiny fraction of the population around me as to have an effect on me very near zero. That’s the usual public good problem.
Insofar as you have an argument, it is that my unselfish concern for other people is a reason to wear a mask, not that my effect on them is a selfish reason, which is what you are claiming.
Even if I have a concern for other people, I also have a very strong concern for myself, so whether the mask protects me is and should be relevant to my decision. Furthermore, whether a mask protects the wearer is relevant to whether I should urge those I care about to wear one, for both their good and mine.
That is a real world issue. In a few days, my daughter is going to do the shopping for the household, being a good deal younger and less at risk than either of her parents. Scott’s essay strengthens the argument for her wearing a surgical mask while doing so. I don’t want her to get sick, and I don’t want her to get us sick.
> If advising other people to wear face masks reduces the risk to me by enough to be worth the effort, then my selfish impulses will lead me to do it.
If those impulses do that for you, good for you. They don’t for kaicarver, whose selfish impulses lead them into the temptation of the availability bias, thinking that anything *they* can do right now, independent of any others, is necessarily the best thing to do. And I think you’re making the same mistake below.
> My guess is that it doesn’t — the number of people I would persuade, if any, would be such a tiny fraction of the population around me as to have an effect on me very near zero. That’s the usual public good problem.
Then you’re trying not very hard? Since I know you’re a smart person, you could come up with something and since you haven’t, you’re not trying very hard. Why not? Because you have fallen prey to the same availability bias trap, exemplified by saying “Scott’s essay strengthens the argument for her wearing a surgical mask while doing so. I don’t want her to get sick, and I don’t want her to get us sick.”
Let me suggest this: have her take a stack of masks to the shop and hand them out (from an appropriate distance), asking everyone to wear them while she is shopping. If you get even 1% of simultaneous shoppers to wear the mask, she’s much better protected than by wearing a mask herself.
I’m sure there’s about 15 other things you can come up with.
Argument by assertion. Would you like to offer some back of the envelope calculations to justify it?
Assumptions:
* we’re talking about makeshift masks (most don’t have decent masks)
* makeshift masks are > 75% effective at stopping spread of droplets in air expelled by wearer (see various links floating around here)
* makeshift masks are < 1% effective at stopping droplets in air inhaled by wearer (that's how I interpret Scott for this situation)
* n shoppers
* base chance a shopper infects you is p (captures how many are infected, their behavior, anything related to how likely they are to infect you)
* all shoppers independent
With no masks, odds of not being infected are (1 – p)^n
If you wear a mask, the odds become (1 – 0.99*p)^n
If 1% of the shoppers wears a mask while you don't, the odds become (1 – p)^(0.99n) * (1 – 0.25*p)^(0.01n)
For p is 0.01 (absurdly large) and 100 shoppers this gives 0.366 vs. 0.370 vs. 0.369
So my 1% was an underestimate: you need to convince 2% to beat the effect of wearing a mask yourself (0.372).
So convincing only one other person to wear a mask confers the same magnitude of benefit to you as wearing one yourself.
For transparency some more numbers:
* If you believe makeshift masks are 10% effective to the wearer, you'd need to convince 14% to wear a mask for the benefit to be larger than just wearing a mask yourself.
* If you believe makeshift masks are only 50% effective to the environment, you'd need to convince 3% to wear a mask.
* If p = 0.001, this whole mask business becomes a lot less interesting, providing only marginal benefits (~0.001 change)
So these numbers are somewhat sensitive to what you believe about the effectiveness of masks and your base chance of getting infected.
If it's a store with 10 people and handing out nice artisanal masks gets 5 to don one, well, that seems like a good trade off to me if you're serious about being afraid of getting infected.
This is kind-of orthogonal to your discussion, but I’d be worried about taking a mask from someone else. If they are an asymptomatic carrier and got virus on the inside of the mask, I’m putting that on my face and inhaling through it, which is pretty much optimal for getting the virus.
Before getting into details …
What you wrote was:
You now have shown that, if you put in a bunch of conjectural values, she is twice as well protected by wearing a mask herself. Note your confident “much better protected” in the other direction.
The mask my daughter will be wearing is a commercial surgical mask, several of which we happen to have. Nothing in our previous exchange implied that she would be wearing a makeshift mask — that was pure invention on your part.
I have no idea where you got that number. Scott cites a variety of different studies of surgical masks. Among other quotes:
All of which suggest an effectiveness one to two orders of magnitude greater than the one you assumed. Feel free to redo your calculations with those numbers.
And very sensitive to the assumption you made that the mask has almost no protective effect, the assumption that Scott just spent a long and detailed post refuting.
Irrelevant to what the policy recommendation is. The correctness of the social policy is independent of whether it’s the wearer or the people around them that benefit. In either case you should equally support things like stores requiring mask use inside or fines for not wearing masks while outside as measures to prevent the spread of infection. So if the question is “should the cdc recommend mask use” whether they protect the wearer seems irrelevant (given a fixed total protection effect size, the distribution of that protection to wearer vs others is irrelevant).
1. Why do you assume a fixed total effect size? One of the things determining the total effect size is whether the mask protects the wearer and by how much.
2. One way of getting people to do something is to show them that it is in their interest. If wearing a mask protects me, that may not be a better reason for you to order me to wear a mask than the same amount of protection for other people, but it is a much better reason for me to choose to wear a mask, given that I am not totally altruistic.
So the CDC is much more likely to have its recommendation followed if the mask protects the wearer than if it doesn’t.
@DavidFriedman
> So the CDC is much more likely to have its recommendation followed if the mask protects the wearer than if it doesn’t.
Saying “much more likely” overstates the case, and even “more likely” is only true if all else is equal. My impression is that you are less influenced by peer pressure than most people, and thus are underestimating the strength of public shaming. If a CDC campaign caused people to shame people who didn’t wear masks in public, people’s desire to avoid this shaming might have an even stronger than self-interest.
Consider the parallel of public spitting. Despite possibly being a benefit to spitter, and despite still being acceptable in some other cultures, in the US it’s strongly looked down upon to spit in public. My impression is that much of the current US attitude is the result of an successful intentional public health campaign against tuberculosis: https://www.mentalfloss.com/article/561579/tuberculosis-anti-spitting-campaigns.
One could argue that this is still the power of self-interest, but it’s the self-interest of those who want not to be infected. If a majority of the public became convinced that their safety was improved by having others wear masks, it seems quite likely that mask wearing could quickly become the norm. If you add in some criminalization or liability for non-mask wearers, the self-protection aspect of masks (or lack thereof) would probably only be a rounding error.
@DavidFriedman
I’m not saying the effect size actually is fixed, I’m saying that the apportionment of the benefit between wearer and others doesn’t matter to policy. Obviously when the benefit is B= X + Y a higher Y increases B, but this article seems to disproportionately focus on Y when X is obviously meaningful and positive so we already know B is meaningful and positive, Y being 0, small and positive, or large and positive doesn’t affect the correctness of a policy of “most people should wear masks”.
Honestly I just don’t believe this. Flu vaccination rates are like ~50%, and it seems very doubtful masks will have a better rational expected value than that. On the other hand, Masks are obvious and visible so a campaign of “people who don’t wear masks endanger you and your children” seems drastically more likely to actually produce compliance because selfish bystanders will help produce that compliance, instead of ignoring violators that “only endanger themselves”.
Is your unstated assumption that as long as B is positive, most people should wear masks, however small B is? Without that your conclusion doesn’t follow, since B+Y could be large enough to justify the policy even if B was not.
Your further argument seems to be:
There are both self-regarding and other-regarding reasons to get flu shots.
Many people fail to get flu shots.
Therefor self-regarding reasons are less important than other-regarding reasons as motives for behavior.
Am I missing something in the logic of your argument?
@david.friedman
Part 1: the context here is basically that the article spends the vast majority of the time on the question of “do masks protect the wearer” when “do masks protect others” is equally important from a general policy perspective (medical personnel/hospitals obviously have justifiably different policies). The only mention of outgoing protection I see is
And by corollary to recommendations to “sneeze into your sleeve” masks seem like essentially a better version of that. Studies that look only at protecting the wearer are going to underestimate total protection from wearing masks and so aren’t asking what’s ultimately the more important question when talking about a policy of “should random asymptomatic people wear masks” (as AFAICT nobody actually disputes them being valuable for medical personnel).
Yes, this is not my argument at all. My claim is that if a central authority gets to make one claim about masks that saying “masks protect others” will reduce in higher mask wearing rates than “masks protect the wearer”, primarily because “masks protect others” spreads itself far more aggressively. “Masks protect others” leads to self interested people demanding that all the people around them wear masks and shaming those who don’t. It’s not about whether the actual motivation for someone to put a mask on is “selfless” (not get other people sick) or “selfish” (protect oneself / not get yelled at). Emphasizing “protect others” also seems more likely to lead to things like stores requiring shoppers wear masks (because more shoppers may demand it as a policy than don’t want to wear masks).
Consider public attitudes towards riding a bicycle without a helmet vs drunk driving. I think drunk driving has a much stronger negative association due to risk-to-others regardless of the underlying actual risks.
The flu vaccine part is a sidenote to establish why I don’t think rational self interest will lead to extremely widespread adoption of medical interventions, even when those interventions have a clear selfish benefit.
If so, it is equally evidence that concern with effects on others will not lead to widespread adoption, since the flu vaccine protects both you and others.
Which was my point.
@DavidFriedman
You’re still not actually engaging with my argument about why I don’t think “the CDC is much more likely to have its recommendation followed if the mask protects the wearer than if it doesn’t.”
I’m saying that “masks protect others” would be a more effective CDC proclamation because it would get people to selfishly make other people wear masks, not that “selflessness” would produce more mask use than “selfishness”. If the CDC tells people that you can wear a mask to protect themselves, selfish and rational people will wear a mask. If the CDC tells people that wearing a mask “protects others” selfish people will make other people wear masks (while presumably also wearing one themselves to not look hypocritical).
A pure altruist should wear a mask regardless of who it protects (because protecting yourself prevents you from spreading the illness as well) so they aren’t really an interesting part of the dynamic.
Maybe our confusion here is on what it means for the CDC to have its “have its recommendation followed”? My understanding of that it’s something like >60% of people wearing masks, and I just don’t see that happening without socially enforced compliance. Because I see socially enforced compliance as being primarily influenced by the degree to which people think “masks protect other people”, I am skeptical that direct self-protection is a significant factor.
Note that one issue with the flu vaccine is that it doesn’t provide very good protection–it’s what we have, but it’s a pretty lousy vaccine. Compare with most other vaccines (MMR, polio, etc.) which are very effective. If flu vaccines were better, it would make both the individual and collective case for getting them stronger.
I mean, my family and I get our flu shots every year, but the protection is better than nothing, and that’s about all that can be said for it.
My claim is that if a central authority gets to make one claim about masks
Why would a central authority with any sense make only one claim? “It’s safer for you and safer for everyone else.” “You’re less likely to get it and less likely to spread it.”
@albatross Where are you getting your “flu vaccines aren’t very effective” information from/what does that level of effectiveness actually mean to you? The CDC reports something like 50% reduction in flu infections and an additional ~60% of decreasing severity in the event of an infection (e.g. ICU rates of hospitalized patients). Neither of those effects is as high as MMR effectiveness, but it feels like underselling it to say they’re only “better than nothing”.
@Roger Sweeny
Obviously the CDC gets to make multiple claims but they have limited time, people have limited attention spans, etc. So their website should always have mostly the full information, but increasing the message length isn’t free, and I’m arguing that emphasizing social benefits is a better use of that budget than personal benefits so it should be spent something like 80/20 on the social benefits. This is in contrast to DavidFriedman who I interpret as saying the personal benefit is more important (but maybe he means they’re equally important and either gets 40% of the population to mask up, this both together is 80%).
But what the CDC has actually been doing is using part of their limited budget of public attention to tell people that there is no private benefit — to lie about the facts.
I assume that both private and public benefit are motives to wear masks. But the CDC never, I think, denied the public benefit, so Scott sensibly focused on the private benefit. That’s important both as one significant incentive to wear masks and as evidence that statements by the CDC ought not to be trusted.
I think the “masks don’t help much” position is common among health professionals in the US. The TWIV guys (academic virologists doing a podcast) have all said the same thing–they don’t think wearing surgical masks does much good at keeping the wearer safe. I suspect they’re somewhat wrong in this case–it probably does some good if only by reminding you not to stick your pen in your mouth or scratch your nose–but it’s not a slam-dunk. For really small airborne droplets, a surgical mask or homemade mask is probably better than nothing but that’s about it. OTOH, it seems really useful for slowing the spread of COVID-19 if everyone wears them, because it seems like most transmission is probably happening from big droplets coughed/sneezed out onto surfaces, and a mask is going to catch most of those. They had a guest (an infectious disease doctor) who more-or-less said that in a fairly recent episode. Though ironically, I haven’t listened to TWIV or other podcasts much lately–that was what I did at the gym, but the gym is closed now.
I doubt that the TWIV guys were worried about causing a run on masks (how many people listen to academic virology podcasts?) and were engaging in a noble lie. I think they were repeating common wisdom among medical personnel in the US, which may or may not be right but isn’t an intentional lie.
There are years where the strains predicted for the flu shot were completely wrong, and years where the flu shot manufacturing was botched up and vastly smaller amounts were produced. If you look at y-o-y flu deaths you could never guess which years those were.
I get the shot, because why not?, but it’s not that great. The people working on it are much smarter than me, that’s not the issue. They are just working on a problem that is much bigger than them.
If you think you can get anyone to wear a mask by telling them it will prevent them from getting infected, you will have as much success as you have by telling them they shouldn’t go the bar tonight.
Many people *have* stopped going to bars and other public places. Not everyone, but a lot of people.
It seems like the only world you find acceptable is the one where everyone wears masks but purely for altruistic reasons. I’m willing to settle for the world where more people wear masks than they do now, even if it is for selfish reasons.
“Confusion”
Nominative determinism strikes again.
Datapoint: My wife and I stopped going to restaurants and coffee shops several days before they were all moved to carry-out-only. The last time we went out to lunch together, the restaurant we went to was almost empty.
@Nathaniel: no, the world I’m going for as one where everyone wears masks. I don’t care about the reasons they have for wearing masks.
I am pointing out that people are misleading themselves by arguments from a naive sense that they are allowed to be selfish, which result in them not sufficiently examining what would be optimal if they truly cared about their well being.
I won’t speculate about the reason for the discrepancy between what they claim to want and what their behavior shows they want, but what would Robin Hanson say?
What do you think the strength of this evidence will look like compared to the evidence for the flu vaccine, which only had about 50% coverage for US adults? It seems far more likely that mask usage would reach high levels due to shaming / social norms which I’d personally guess are easier to form when not having a mask mostly endangers others.
This is also my takeaway. I’m a reasonably young, reasonably healthy person (at least as related to COVID-19 risk) living in a large multifamily building with many older and less healthy folks. It sounds like making some sort of fabric mask from an old pillowcase or whatever is unambiguously the correct thing to do, and the rest of the post is interesting but for me, not actionable. I wish my home’s craft supplies were better stocked.
I agree. There are a lot of DIY mask tutorials out there by now. Some use very little craft supplies, for example, I’ve used stapling instead of sewing and it works just fine.
However, WHO says:
I wonder why is that.
I assume it’s a “not recommended” vs “recommended against” thing, but I’m confused on why they don’t word it as “only minimally effective” if that’s the case.
coming from hong kong where the topic of masks has been discussed at length over the past couple of months, here are some things we’ve learned:
– wearing a mask is a good idea if supply for healthcare workers is not a concern. this is especially important since asymptomatic covid carriers abound (and hong kong is a dense city). another upside is that it encourages those who are sick to wear a mask without the fear of being identified or stigmatized, and in turn becoming unknowing transmitters.
– for diy masks to be meaningful, they need to mimic the protection of surgical masks.
typically, a three-layer surgical mask has a waterproof outer layer, a middle layer that filters tiny bacterial and viral particles, and an inner layer that absorbs the moisture exhaled from the wearer. both the outer layer and the inner layer are to protect the middle layer from getting wet and becoming a conduit for bacterial and viral particles to pass through, defeating the purpose of the mask.
therefore, diy masks would need to be able to keep the filter cloth dry for it to do its work. one way of doing so, though un-elegantly, is to wear a full-face visor at the same time and adding a tissue between the mouth and the filter cloth for moisture absorption. the filter cloth can’t be too porous either, otherwise the tiny viral/bacterial particles can still pass through.
– as another commenter suggested, having a mask on helps keep people from touching their faces, which is important as well.
so, if masks are available, by all means wear one. or make one that works well.
Would a single layer of cloth help reduce an infected wearer infecting others?
for an unknowingly infected person, a cloth mask may reduce droplets from spraying all over during coughing or sneezing, but it may not be enough to block covid droplets given their minute size. some people who make diy cloth masks insert a piece of non-woven fabric (like a dried wet wipe or even an air-conditioning filter) in between cloths as the filter to mimic surgical masks. that seems like a better option.
separately, the WHO has published some guidelines on mask use that is a good reference:
https://apps.who.int/iris/rest/bitstreams/1272436/retrieve
Yes!
1) Almost any mask will create turbulence and therefore prevent your breath from spreading as far, generally. This is a Big Deal.
2) Almost any mask will serve the crucial role of interfering with coughs and sneezes (which can literally travel 20-30 FEET!)
3) Most fabric masks will catch the largest droplets (which contain the most virus and are the most dangerous) and
4) Most masks have a psychological aspect which may keep you focused on transmission issues.
FYI: If you really have to cough or sneeze and you’re not wearing a mask, the safest way to protect those around you is NOT using your sleeve. It’s to pull out your neck and sneeze/cough down your shirt. Yes, it’s a bit gross but is highly effective.
Thank you, this makes sense.
“People may get infected by the virus if they touch those surfaces or objects, and then touch their mouth, nose or eyes.” (from covid19.govt.nz) – does that imply that to be completely effective a mask would need to cover your eyes as well as your mouth and nose? Or is direct contact infection significantly different from aerosol infection?
If it’s a true aerosol situation, you’d want a full face respirator.
If it’s respiratory droplets, but you’re worried about it getting in your eye/nose, you can wear a mask under a face shield.
As long as you don’t touch your face, a mask should protect against respiratory droplets just hanging in the air/directed towards your mouth.
On the ambulance, we have PPE kits that comprise a respirator, a face shield (to protect the eyes), a gown, and gloves.
But that only protects against droplets, not airborne risks for which you would need a CBRN mask (also currently sold out).
This post correctly notes that there is a nationwide shortage of N95 masks. Most worldwide supply is currently spoken for, though production is rapidly ramping up.
But it may surprise you (or may not, depending on how much pre-existing cynicism you have about the regulated nature of the healthcare industry) that there are millions of *exactly equivalent* masks sitting around, in stock, ready to be bought, that are not being utilized. These are “KN95” masks. These have basically identical specifications, here is a writeup by 3M: https://multimedia.3m.com/mws/media/1791500O/comparison-ffp2-kn95-n95-filtering-facepiece-respirator-classes-tb.pdf
KN95s and N95s are in fact, often manufactured in the same factories. But the difference is that production of N95s are ceritifed by the US FDA, whereas production of KN95s are certified by the equivalent Chinese regulatory agency. This detail makes no difference in how well the masks protect against COVID19, but ensures that essentially no hospital in the United States can buy them. CDC just issued guidance last week recommending that hospitals consider masks of equivalent international specifications: https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/crisis-alternate-strategies.html, but I have yet to encounter a single hospital purchasing department that has adapted to this recommendation.
The N95 shortage is so acute that I have heard stories of nurses, sometimes over 60 years old and vulnerable to COVID19, going into ICUs to treat confirmed COVID19 cases with only a surgical mask. Or with a single N95 mask that they re-use every day (official guidance is to swap these out after every *patient*), despite no clear reliable way of sanitizing them.
The shortage of N95s while millions of functionally-identical but legally distinct masks sit in warehouse struck me as so galling that I decided to just raise money to buy KN95s from China and then distribute them to US hospitals, usually giving them directly to doctors and nurses since the hospital administration officially deals just in FDA-approved equipment. I apologize for probably breaking some rule about promotions and perhaps getting this comment deleted, but I’ll risk it because this is worth it; you can donate here: https://www.gofundme.com/manage/kn95-masks-for-impacted-hospitals . I have so far raised enough to order 60,000 masks and, if I just had the money, have the ability to purchase many hundreds of thousands more.
I am effectively doing the exact same thing for the exact same reason. I have several sources for KN95’s (which Scott should address in this post) and am buying and distributing as much as I can. My company is going to do a “Masks for All” coin as a fundraiser (we make coins/belt buckles usually). We’ll sell you a coin and buy several masks with the proceeds and distribute them. I learned about the differences on my many trips to China over the years and couldn’t believe that during the present shortage, many hospitals would rather reuse (without sterilizing) K95’s than use KN95’s. It has been my personal online crusade on Facebook (ugh) trying to convince people that the masks that are 3X less expensive and readily available are likely as good or at least ALMOST as good as the ones that no one can get.
Also look for R95/R100 and P95/P100. I’ve had luck finding those even while the N95 masks are months backordered. I’d much rather wear a P100 than an N95 for virus protection
Yeah, it seems a lot easier to get the seal to work on my P100 mask than on the N95 mask I wore to the store last time I went. I may just go with the P100 mask next time, though it will look extra weird. I guess I’ll wipe off the surfaces with a disinfectant after going out with it.
I think you’ve put in the wrong link – https://www.gofundme.com/f/kn95-masks-for-impacted-hospitals works for me (note the “f” in place of the “manage”).
Thank you for the correct link, I may have given up otherwise!
argh, thanks so much for fixing this!
I am donating today. Please update when you have begun distributing masks and confirm that healthcare staff are using them and report what your turnaround time is from purchase until the masks are in use. I’ll likely make another donation at that point.
If anyone else has commentary on why we should or shouldn’t donate here, or a recommendation for a more effective donation, please post!
Thank you very much! The first shipment will arrive Friday or Saturday, and I will be sending an update to the page when this happens.
I think this is at least partially inaccurate. Here is a great summary from a LessWrong thread: https://www.lesswrong.com/posts/7K8fSFTnpfN4EBuZ8/how-useful-are-masks-during-an-epidemic?commentId=DAJTniy2swhdtiZdh
Hey there –
I admit I’m not an expert on industrial mask design and can’t address all the specific engineering points. But I have learned a few things from my research talking with both physicians and medical import/export companies.
– “industrial vs. medical” is orthogonal to “KN95 vs N95”. There are industrial grade KN95 masks and medical-grade KN95 masks, just as there are industrial grade N95 masks and medical grade N95 masks. Of course, medical-grade KN95 masks are pretty much only sold and used in China. I’m just speculating here, but maybe US industrial users routinely buy KN95 masks because they are a bit cheaper, whereas hospitals never do, which is why the commenter thinks all KN95’s are industrial-rated?
– Note also that FDA just issued guidance last week for hospitals to go head and use industrial-grade N95 masks if they have to, extending liability protection to those manufacturers.
– the point this comment raises about moisture is absolutely true, and common to hardware-grade masks of both the KN95 and N95 varieties. It’s definitely a compromise that is being made with the short-term use of hardware-grade masks in medical settings.
– fit is also orthogonal to the KN95 vs. N95 distinction – there are masks in both categories that either have multi-size fits or attempt to be one-size-fits all, the former being better and safer but, of course, requiring you to track and order multiple SKUs.
Hi @mlinsey , we have a few nursing homes which need masks, and may be interested in buying if they can arrive fairly quickly.
How can I get in contact with you?
Scott please delete this, thank you
Over here in East Asia, it is generally believed that one of the main benefits of mask use is that is stops people from touching their face, nose, and mouth (this is critical!), in addition to the limited protection a mask itself might offer.
And the common wisdom over here is that surgical masks work. Period. The government wants everyone to wear a mask, even if you have to put it on a clothesline for a day after use. Which is why… I found the the back-and-forth in the US rather amusing.
It is not improbable that the CDC foresaw the possibility of future shortages of medical equipment, and intentionally geared their policies to prevent excessive demand three years in advance. After all, all these pandemics aren’t exactly super-unprecedented, and well, everyone knew this sort of thing could happen.
I don’t find the situation in Asia very compelling evidence. That is, it’s just as likely that east Asian society is blind to scientific fact as that western society is.
In particular, isn’t mask-wearing pretty common in east Asia for reasons unrelated to germs, namely seasonal dust storms (so I’ve heard, unconfirmed)? That would reasonably bias people to support evidence that masks have other positive effects, since they’re wearing them anyways so it’s low risk.
Lots of mask use due to scooter use and general traffic congestion, but also superstition after SARS. Well superstition is a strong label, people just accept it because it has become the norm. But the rationale that made sense to me is that covid19 spread via respiratory particles, and mask reduce the viral load over time, which reduces risk of infection and severity since your body will have more time to recognize the infection and ramp up antibody production much earlier in the virus’s exponential growth cycle. Reduces R0 when ubiquitous, almost like cheap heard immunity.
I think the country to observe is Japan, fairly ubiquitous mask usage, by all accounts they’re under-testing to suppress numbers so Summer Olympics doesn’t tank (except it just did), but also they should have been overwhelmed like Italy by now, that level daily death – military trucks convoys shipping coffins – can not be hidden. Instead, ground reality doesn’t appear starkly different than Korea or Taiwan. I think there is a chance that China over reacted because it had to, there was so much unknowns early in the outbreak. But seems like all the countries that are doing well right now have ubiquitous mask usage and hygiene due to past SARS experience. That or because they’re functionally islands and can easily shut down their borders.
There are far fewer cases and deaths in Japan now as compared to Europe despite the disease having arrived there earlier and the fact that life has shut down to a lesser degree with people still riding crowded subways, etc. Of course, other factors could contribute (bowing instead of kissing on the cheek), but it makes sense that if it’s spread by coughing, sneezing, etc. widespread mask wearing would significantly slow the spread even if not that useful for each individual.
I think mask wearing is more or less ubiquitous in SE Asia, and that is where you find the countries that have been able to curb the pandemic. This is circumstantial evidence, but it is one more thing to consider.
Actually, people wear masks during exam season, so their performance during and immediately before school exams doesn’t get screwed over by a cold or something.
Some people wear masks when air pollution is particularly bad, but that isn’t common at all.
All sick people are expected to wear masks in my corner of East Asia; to not use a mask while obviously sick is considered very rude.
And as usual many Americans and Euros in East Asia don’t wear masks even when available and walk around scaring the bejesus out of the rest of us.
This does not match my experience with face masks. I wore a face mask last time I was sick, and I felt like I touched my face more often, in order to adjust the comfort level. I suppose I might have touched my mouth less often, but nose and face seemed to be very often. Maybe I am just atypical and was doing it wrong?
I had the same problem initially; I also found it difficult to breath at first. Somehow you get used to it and it doesn’t seem so bad. That said, while it may possibly be a wash in terms of risk for many individuals (lower chance of inhaling virus offset by higher likelihood of touching your face to fix your mask or feeling of safety conferred by the mask causing you to be less cautious in other ways), I’m pretty confident it’s highly beneficial when almost everybody using e.g. public transportation is wearing. Imagine how many people could get infected by one uncovered sneeze on a crowded subway; not just because they might directly inhale, but because the saliva can alight on surfaces people will touch.
It seems to me that respiratory viruses have clearly evolved to take advantage of our bodies’ reflexes to expel crap from our respiratory systems by coughing and sneezing. That’s how they get a free ride to the outside, and from there to other bodies, either directly or by landing on something people touch. Effectively covering everyone’s coughs and sneezes in public seems to throw a major wrench in that.
“amusing” is one way to describe it. I would describe it as infuriating and terrifying. I feel like western society is too disorganized and selfish to get this thing under control any time soon. It seems like it’s going to just keep spreading until half of us all get sick, one way or another.
Here’s some top Korean doctor on infectious diseases saying masks are effective and that he’s not sure why the CDC saying differently except possible because of trying to prioritise masks for medical staff
https://youtu.be/gAk7aX5hksU
In Japan many people wear masks for hay fever.
https://en.wikipedia.org/wiki/Hay_fever_in_Japan
For what it’s worth, Chinese National Health and Medical Commission recently posted their official guidance on mask usage. The cat meme is because someone reposted the article on Chinese Quora. Use Google translate. Normal surgical masks is recommended for almost all circumstances N95+ for specific personal and exposure. The only situation where no mask is necessary:
Also, relevant interview with microbiologist Yuen Kwok-yung, “key figure in identifying and arresting the spread of the Sars pathogen that ravaged Hong Kong in 2003”, and one of the expert group who was sent to Wuhan at the beginning of the outbreak:
Give
+1
The burden of proof is on organizations like the CDC telling people that wearing masks is “not recommended”. Unintuitive advice requires justification, since when none is forthcoming, credibility is diminished.
If there is a well-founded concern about supply, at the very least you would think that DIY masks cannot hurt, so you might as well wear them. Again, one can imagine reasons that this might not be the case, but the burden of proof lies with those imagining such reasons.
“Not recommended” doesn’t mean “recommended against,” does it?
This was Scott’s point here:
Indeed, I thought to comment on this. However, there is a reason that containers full of petrol are not labeled inflammable.
Consider not wearing a mask when driving (they can be distracting), especially an N95+ mask which can make breathing more difficult.
“When used correctly, they[respirators] theoretically offer complete protection against incoming and outgoing droplet and airborne diseases”
“Also, even respirators don’t claim to reduce particle load by more than 99% or so, and those work”
“But it would also be wrong to conclude the studies show masks don’t work, because they mostly show respirators don’t work, and we (hopefully) know they do.”
99% isn’t complete protection. Complete protection hasn’t been demonstrated, so “theoretically” is meaningless. But “we know they work” seems to depend on complete protection, or on the hope that a 95-99% reduction is enough to let our immune system do the rest – which may be less true for some viruses, perhaps especially for novel ones.
I think probabilistic elimination of viruses confers protection regardless. If 1 virus is enough to get sick then 95% won’t do much in a 100 virus environment, but will probably protect you in a 10 virus environment.
I think there’s also some complicated biology things where case development can differ based on number of viruses in the initial exposure – see e.g. https://ccforum.biomedcentral.com/articles/10.1186/s13054-019-2566-7. So getting 5 virus instead of 100 may lead you to still get infected but have milder/no symptoms.
If the anecdotes about many deaths in the medical profession are true, it seems quite likely that the number of virions you are exposed to counts.
I suppose it might also depend on *how* you are exposed to them. What if ingesting some viruses to your digestive system might let your immune system get acquainted, whereas they only do harm when they get into your lungs? (Purely speculative hypothesis.)
This seems awfully likeky to me too–young, healthy healthcare workers might not get badly sick if they rode the subway next to one sick guy once, but spending 12 hours a day in a roomful of very sick people, sleeping on a cot in the hospital and reusing their mask/gown the next day to conserve supplies, they’re getting a ton of virus exposure, all the time. Also probably getting many slightly different strains of the virus at once, which might matter.
Robin Hanson is speculating along these lines and has some additional studies where initial dose seems a strong determinant of long term outcome. The home vs public exposure piece is very speculative though, it’s not clear how it changes if the larger dose comes cumulatively over a 24-60 hour period.
Anecdata: A few years ago I had to work with smelly hot plastic. No protection was required, but I got a respirator and wore it with a short beard (obviously knowing it was not properly sealed). A significant amount of air went through the cartridges, and from the reduced intensity of smell, I’d guess that it filtered about 75% of the air I breathed.
My face was sweaty so I could sometimes feel air slipping past the plastic near my nose (where the beard wasn’t). So I can confirm that even with no beard (and no training or fitting), if I’d needed protection from a really deadly atmosphere, I’d have been dead. But if I just needed a 10X reduction in the bad stuff, I could shave, get a Home Depot respirator and good cartridges, experiment with fit by covering the intake holes and adjusting until I couldn’t inhale, and probably be OK.
I’d guess the sense of smell isn’t linear with particle density. So filtration was probably around 90%, if it felt like 75%.
Yeah, I’ve worn Home Depot respirator masks to deal with stinky organic waste, and it took the smell down from can’t-approach-it-without-gagging to barely perceptible. If these things successfully protect you while sandblasting black mold off a house frame, and can block out poo smell almost entirely, surely they’ll at least help against globs of spit floating in the air?
Problem is nobody in those studies wore a Home Depot respirator which seals WAY better than this N95 one way crap. Why this is is beyond me.
Wouldn’t western culture’s strong tendency towards individualism make the broad population incredibly likely to risk-compensate a lot, thus making a large-scale mask-wearing intervention counter productive? This is a very pessimisstic idea, of course, but could enable a charitable reading of the CDCs policy (and even explain the contrast to asian countries’ policies to a certain extent).
I feel your pain. In Army basic training, they gave the standard two minute explanation, made you put your gas mask on, and made you stand in a cargo container with the rest of your platoon where they threw in a CS gas grenade and shut the doors. Then they made you jump up and down and sing the Army song. If you began to cry, vomit, and leak profound amounts of snot out of your nose while struggling to breath and feeling like you just ate a really hot chili pepper with your entire face, your gas mask was leaky and you failed.
Only a handful of people in my training platoon of 50 completely lost their shit, so anecdotally gas masks are easier to figure out than N95 masks. I imagine gas masks are pretty useless for health care providers, because wearing one while moving around and working is exhausting for any length of time. They might be OK for quick trips on the bus though.
On the subject of masks, is anyone else infuriated that the US is apparently so far down the path of decadence and decay that we as a nation can’t figure out how to mass produce and distribute a simple fucking fabric rectangle with ear-loops?
I remember this from basic. I could be remembering wrongly, but didn’t we also have to take the masks off and just sit in the gas for a bit (breathing and feeling it) – just to know what it felt like? I remember going in, putting on the mask, getting gassed, then being told to take off the masks and “experience the gas” – this was almost 20 years ago, so I could be wrong.
That’s how it was for me (Navy basic training in 2004).
You go in the room, and put your masks on. Then they release the chemicals. If you did it right, you’re fine and you don’t notice anything. They help the people who did it wrong get theirs fitted, then wait a bit. Then, one rank at a time, you have to remove your mask, stand around a bit, and “sound off” (name, rank, serial number I believe). Once every person in the rank has completed that, your rank is dismissed.
Gas mask training was my favorite day because everybody got to feel their mucus membranes start to vent everything while a sergeant screamed at them that they were screwing up things that a baby could do right.
If you can properly adjust PPE in that circumstance, anyone can learn to do it.
Marine Corps, 1986. Crusty **OLD** Master Gunnery Sgt. takes off his mask, stows it in the carrier, pulls a pack of Chesterfields out and lights it. Half the rest of the room is gagging and coughing and snot’s pouring out of their orifices and he’s completely NO FACTOR.
“On the subject of masks, is anyone else infuriated that the US is apparently so far down the path of decadence and decay that we as a nation can’t figure out how to mass produce and distribute a simple fucking fabric rectangle with ear-loops?”
No, because the framing is totally wrong.
Consider the runs on grocery stores. We’ve had people buying out costco like maniacs, yet we don’t have canned food shortages…the next day, you go back to the store, and the empty shelves are full. Why? Because current demand is not dramatically higher than normal demand, because people aren’t actually consuming more food than normal. Sure, they’re stocking up, but not on a scale that vastly exceeds normal variations, like holiday seasons. The system has plenty of slack capacity and demand isn’t outstripping it.
Now consider the market for masks. Western societies don’t go around wearing surgical masks as a matter of course. The only people that use them are doctors. So the market is set up to meet the demand that DOCTORS have, say during a bad flu season, plus ten percent. But that supply chain cannot possibly supply a 100 fold increase in demand, and it’s uh unlikely to ever tool up to meet it, given that after this is all over, nobody is going to be wearing masks and all the new mask factories will default on their loans. Compare this with east asia, where masks ARE a daily part of life, such that current mask demand is not that much higher than normal mask demand, and you can tell the whole story about masks without maudlin characterizations about decadent modern society.
Yeah. It’s ironic, but better organized supply chains means less stocks mean less reserve in an emergency. And from what I read a good supply chain is what makes or breaks a modern company.
The same efficiency means that the bounce-back should be rapid and complete, but… not from day 1. It takes a while to ramp up production.
This is what could have been helped by the government. Smart people should have talked to production companies and convince them to build up stocks. If necessary, they could offer a guarantee to buy those stocks at current prices, if the crisis doesn’t manifest. This should be standard practice – but it probably isn’t. (although I’d bet a fingernail it is standard practice in at least some Asian countries. Half a fingernail if Japan isn’t one).
Taiichi Ohno’s ghost is laughing his ass off right now
The government “stockpiles” all sorts of “strategic materials” so they have them in a crisis. With 20-20 hindsight, a stockpile of masks should have been built after the 2009 H1N1 flu.
Google led me here which suggests in 2009 there were already considerable suppliers, both of antivirals and of marks. Not sure what was the situation now. To note that the dimension of the problem we have now is not one likely to be considered reasonable back the. “Enough masks for the whole population to wear continuously for 6 month” sounds like an exercise in finding the upper bound, not a real life number. And the costs are probably similar.
There are worse situations. Our old Govenment (Romania) left us with no emmergency stocks whatsoever, and with a system of price ceilings for drugs, possibly the lowest in Europe. So the problem isn’t that “my lifesaving drug is expensive, I’d better get some help from the state to compensate”. It’s “my lifesaving drug is so very cheap money’s not even a problem. A lot less then a plain ticket to Vienna where I can actually find it in a pharmacy”. That last one wasn’t a zinger, people are actually left without life saving medication and resort to all sorts of complicated ONG networks to get them imported (obviously at unnoficial prices).
In all fairness, the new Gov is showing the proper distaste for the situation. Not sure why they’re not using the emmergency situation to get rid of price ceilings – hope it’s not electoral reasons, but it probably is.
I can’t source the claim right now, but I’ve read that there was a stockpile of masks before then. It was released for use during the H1N1 flu and never actually replenished.
@Dissonant Cognizance
I’ve seen this one.
Another consideration: we used to make a lot of masks here, and now we don’t, because it’s cheaper to produce them in foreign countries. This story talks to a domestic mask producer which described the switch:
However, when the Rona came, the East Asian producers clamped down on exports leaving us with just our domestic production. Note that I don’t blame them for this–if we had to halt exports to take care of Americans, I’d be on board with that, and I expect other governments to do the same.
As an aside to my main point, the mask producer in the article (Prestige Ameritech) almost went bankrupt in exactly the way you describe during the swine flu outbreak:
That helps me understand the situation better, thank you. Perhaps when this crisis is over, in addition to stockpiling masks, the government should stockpile a few dozen of these machines.
According to https://www.washingtonexaminer.com/news/los-angeles-times-and-bloomberg-news-federal-stockpile-of-n95-masks-was-depleted-under-obama-and-never-restocked
The US had a national emergency stockpile of N95 respirator masks from 2005. The stockpile was depleted during the 2009 H1N1 outbreak, and was not replenished. You can’t blame that one on Trump, although I suppose if he were really on the ball he could have reversed the decision made during the Obama administration to let it slide.
For any healthcare workers affected by the mask shortage, this report on mask reuse and other related topics from Stanford is useful: https://stanfordmedicine.app.box.com/v/covid19-PPE-1-1?fbclid=IwAR25akR3mlhjyUZJ8RiaBxRBr38YxXgOuF00hFzh5zbfPadaWWDehNt42W0
Some interesting tidbits:
– You can disinfect facial masks for reuse in an oven at 70 C for 30 min or steaming it for 10 minutes
– If you’re gonna make your own mask, a vacuum cleaner bag is the best material, followed by a tea towel.
Speaking of which – would it help to run air condition (if it is HEPA-filtered) to remove floating viruses/droplets/aerosols? Other ways to filter the air?
For aerosols it would probably help a bit – at the very least, they use HEPA filtered air for people undergoing immune depleting therapies, so they should be quite good at removing viruses from air. Obviously aircon is going to be less effective than a specially engineered room. And you still have to deal with droplets on surfaces.
The table of mask materials seems to be based on this paper:
https://www.researchgate.net/publication/258525804_Testing_the_Efficacy_of_Homemade_Masks_Would_They_Protect_in_an_Influenza_Pandemic
The table of materials summarized in your link, in the original also includes values for pressure drop. The materials with high filtration effectiveness are vacuum cleaner bags and doubled tea towels, however those materials also have much higher pressure drop than surgical masks, making them significantly more uncomfortable and tiring to wear.
I would be curious to know whether anyone here has tried a vacuum cleaner bag mask and how heavy the penalty is in practice. The paper cited above does not give a pressure drop figure for N95 respirator masks.
The summary:
As other commenters have pointed out, the big benefit of masks is that, when everyone wears them, symptomatic or not, it dramatically reduces the spread of respiratory illnesses. I’d like to quote this article for some further commentary:
It seems the reason why exposure dose matters is that when you are exposed to a small dose, the virus needs more replication steps in the body until it reaches a number where it overwhelms the immune system. This buys the immune system time in which it can start to fight the virus.
> Remember, there are dozens of studies supposedly showing homeopathy works, not to mention even more studies proving telepathy exists.
But homeopathy does work, and telepathy does exist. Masks and respirators work for precisely the same reason as homeopathy, which is the same reason that many cancer treatments work. Using a mask reflects a decision on behalf of the wearer to not get sick, and serves as a constant reminder of that decision. The wearer asserts control over the outcome (I refuse to get sick), as opposed to the non-wearer who believes they are subject to the whims of randomness (it is not in my hands whether I get sick). Therefore more non-wearers get sick because they convince themselves they’re not in control of their own experience.
See The Nature of Personal Reality (a Seth book). Reality is not linear. Chasing studies is chasing your own tail because the studies show you what you want to see. You do not perceive realities where outcomes are different. Other versions of you experience those realities, reflecting what *they* want to see.
Are you claiming that wearers, believing that their health in their own hands, practice better hygiene in general (wash their hands, socially distance, etc) leading to lower infection rates, in contrast to non-wearers who don’t bother? Or are you claiming that simply the act of believing one is in control will, in and of itself, affect one’s probability of being infected?
I think he’s saying that “in and of itself” is a fallacy. We’re not spherical frictionless objects in void. The act of believing something affects your reality in some way.
It’s pretty clear there are confounders between:
a. Compliance with mask use vs doing other things like washing hands properly and doing proper social distancing.
b. Having a mask on vs remembering you’re supposed to be being careful.
c. Having a mask on vs signaling to other people that you’re either sick or taking social distancing seriously.
OTOH, you can believe you are immune to a disease and still catch it, and there are plenty of worked examples of this.
It seems like the latter. “The Nature of Personal Reality (a Seth book)” looks like metaphysical woo where believing you can get sick itself contributes to the probability of becoming sick by metaphysics and/or magic.
I’ve read a lot of studies with conclusions I did not expect — or, sometimes, want.
I liked this study, which tested things like a pillowcase, a cotton t-shirt, and a vacuum cleaner bag. They all do some work, though not as good as a surgical mask.
A tangentially related question. I’ve heard two Covid-19 scenarios discussed: (1) social distancing etc buys us time to flatten the curve and develop treatment options. Everyone seems to agree this would require very long and stringent social distancing with severe economic impact; (2) testing and quarantine allows us to reduce transmission rates and stamp out the disease. This is a much more optimistic scenario. Can anyone recommend / provide a good analysis of how plausible scenario (2) is? Most of the discussions of (1) implicitly assume that (2) is not plausible, but without addressing it directly.
These options are time- and path-dependent and contingent on having the requisite capacity. You do (1) after you’ve not acted quickly enough to do (2). Doing (1) instead of (2) when both options are available is bad.
(1) is also on a spectrum, where the degree of social distancing can be extreme (no one leaves their homes; everyone wears masks when they’re out) or mild (what most of the US is doing now) and complied with to varying degrees. (In Wuhan, high compliance for various reasons. In the US, variable compliance across jurisdiction.)
In our current case, we could’ve done (2) effectively in Jan/early Feb if we’d acted much faster to get testing set up. So now, my hope is that we’re trying to do (1) over a short(ish) horizon so that we can build up adequate capacity to start doing (2). But AFAIK, we don’t have a clearly articulated long-term plan, and in the short term, we’re focused mostly on (1). I also don’t think we’re doing (1) stringently and consistently enough to transition to (2), but hope springs eternal.
If we could keep most of the country in social-distancing mode for, say, 4-6 weeks, we will *massively* slow the spread of the virus. It will die out in some places where it’s spreading in the community. Add to that some kind of well-thought-out strategy for keeping healthcare workers and family members of sick people from spreading it, and we could actually end up with a lot fewer cases to deal with–hopefully enough that we can go back to what we should have been doing intiially–tracing each known positive case and all their contacts, isolating them, etc. Add to that some less disruptive level of lowering the expected number of new cases caused by each infected person (masks, social distancing, wiping everything down with bleach every few days, maybe summertime coming along and making the virus break down faster on outdoor surfaces), and maybe we can keep ahead of it this time.
Hmmm. New Zealand was doing contact tracing and isolation from day one, and we’ve still wound up going to lockdown due to community transmission (i.e., people who got the virus and we can’t figure out how).
We weren’t wearing masks though. Perhaps that would make enough of a difference, I dunno.
I wonder if we will see a permanent shift to more delivery/car pickup shopping as a result of this pandemic.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3004550/?fbclid=IwAR0kCXky8BshUdkFSyR4Rcku12eMmfvtDX3wId4urd5uXHiRmbqVP3OTcLw this post-sars paper strongly recommends facemasks. “Experimental results showed that when droplets spread onto a person face-to-face over short distances, 92.3% to 99.5% of droplets were blocked by the front surface of the facemask, whereas only 0.5% to 7.7% of droplets reached the back of the facemask. Both facemasks A and B had near or over 99% protection efficiency, compared with that of 95.5% to 97% of surgical facemasks.”
But maybe this is in the above mentioned controversial category?
At least in Italy, there are lots of people wearing them leaving their nose uncovered, actually.
That seems like an easily-correctible error. Giant PSA and statements from the people giving speeches that masks must cover your mouth and nose.
I work in a retail pharmacy in California and have already seen every possible way someone can get surgical masks wrong: nose outside mask, mouth outside mask, mask being worn under chin, mask with only one loop attached and dangling, one woman not wearing it and just straight carrying it in their hand, plus several people who would wholesale take them off as soon as they had to talk to someone. Definitely one of those things where if you think it’s foolproof you might just be lacking in imagination.
Even in East Asia at least 25% of people get it pretty wrong. The nose thing is the biggie.
Eh, this does not follow. An airborne virus is small, but much, much larger than an air molecule, aerosol droplets are even larger. In addition, there could be electrostatic or other effects, helping to entangle pathogens.
And even if they let through some viruses, this is not the same as “offering no protection” against disease.
I assumed that by that he meant that gaps on the side of the mask allow air to reach the wearer without passing through the mesh of the mask. I think if 100% of breathed air went around and through those gaps there might not be airborne protection, but I think some still passes through the mesh of the mask to provide partial protection for the reasons you say.
I am middle aged with a heart condition. I have a suspected Covid patient in the house in quarantine— test still pending but fever, cough, sneezing and back from hot spot. Where can I get surgical masks?
This is advice for where to look for things that are equivalent, since that’s what I’ve been doing. Surgical masks are commercially unavailable where I live right now, at least on time scales that would be good for you.
The hardware store. Or the auto parts store. Respirators and masks sold to keep you from dust inhalation or fume inhalation are definitely better than nothing, and people don’t think of them as readily.
The disposable gloves they sell for use changing oil and other such purposes are also very useful – they’re heavier and bigger than a lot of surgical gloves, which means they’re washable. Plus, by wearing them I can spray my hands with disinfectant when I spray the grocery store cart.
Often they’re better than the N95 masks, in fact. Some time ago I picked up a P3 mask for home repairs (European standard, to filter 99.95% of particles and functionally equivalent to N100 [99.97% filtration]) for around £30.
Sadly that was a while ago, the filters have long since expired, and I can’t get replacements for love nor money (to be fair, I haven’t tried offering love, only money…)
Are any kind of masks available commercially?
About a month ago I did a low-intensity search at Lowes and Home Depot and found none. I didn’t try super hard digging everywhere I could.
You need to be a big player with a contracted supplier, buy from the black market, or get/make a homemade one.
Note however that if the intent is to have the suspected patient wear a mask, you need to make sure the outflow valve is kept closed, as it bypasses the filters.
Tape would be the obvious solution, but I’m not sure I’d trust tape given the level of moisture that would build up. Rubber cement would be effective, but would take some time to dry sufficiently to not cause issues with fumes.
Might be best to have everyone else wear a mask instead.
See this link from above in the thread on how to reuse/make masks:
https://stanfordmedicine.app.box.com/v/covid19-PPE-1-1
Try paint shops, the full face and cartridge respirators may still be available.
Thanks for all your responses. We were able to get some disposables from a friend and sew some others. How the patient tolerates mask wearing remains to be seen.
… And what I took away from this is that someone really, really needs to design a n95 mask with a more reliable and universal fit, and ease of cleaning.
Uhm. That.. actually does not seem that difficult, even given the requirement to keep cost down. Hat with all the filters and valves in it, transparent plastic veil 360 degrees hanging down from the brim, seal it around the neck. The neck being a pretty good approximation of a pipe with no significant hair on it, that should work, and there is more or less no way to wear it wrong. Yes, I realize this amounts to wearing a plastic bag on your head.
Snorkel intake? Nah, pipe to noseplug. That way you can talk..
Uhm. I need a 3d printer, some sillicone tubing and some airfilters.
You need to be able to remove a used/contaminated mask with minimal skin/orifice contact. Slipping off a turtle neck will smudge contaminants all over noses and eyes.
I think the lesson is to keep a huge contingency stock, Canada just found 55m expired n95s from SARs response, that was validated fit for use. But it seemed like they were just lost in the system. Also reshore essential manufacturing, even if sunk cost. It doesn’t even have to be military industrial complex level where plants make a few tanks every year to retain personnel. But just have the equipment ready to spinup and enough PPEs to last 3-4 months it takes to setup production lines.
Also n95s are like… the minimum protection equipment in these cases. Really every doctor and nurse should have a hood respirator, if only in storage. I’m guessing the military has enough gas masks.
If you want to look at somewhere obvious to improve, apparently one of the largest expendidure of PPEs is sadly… adjusting settings on ventilators next to patients because they’re not wireless :-/.
E: Also I think when this is over, every individual should stock some just in case. Hell everyone should have a PPE set ready to donate incase of shortage because institutions and cost savings have short memories.
Not a turtle neck – the plastic sheet you see through is a straight tube, cinched in around your neck under your chin and at your collar. Take of the cinches, you can just lift it straight up and throw it in a boiling pot. Currently playing with 3d maker software, the hat part needs to be something which can be spat out of a die in a plastics factory, and its been a while since I did anything like this..
Doesn’t even need to be wireless, the wires could just be long, right? Like if the wires fed to a control panel outside the room you don’t need to worry about theoretical wireless communication interference/security risks (though in turn you need an air tight seal for the wire to pass through).
Are respirators really that hard to use? I picked up a P3 half-mask (one of these) for painting and decorating the house ages ago and adjusting the fit and testing it was the easiest thing in the world – put on head, tighten straps, cover filters and check you can’t breathe, pretty much.
I think he’s talking about N95 disposable masks.
“Cover” hides an issue though, as it’s easy to “cover” with enough force that you fix a poor face seal for the duration of the test.
I respectfully disagree with this. Contingent upon how exactly you define “hoarding.”
How could you disagree with this? Masks are already in desperately short supply in many US hospitals, and we really need hospital workers not to get sick en masse. Given that, I don’t see how most private individuals can justify keeping any masks for themselves right now.
Question: I have a face mask respirator that’s intended for industrial/commercial use (it’s from chemistry lab when I was in school). Would that provide protection? I was thinking of giving it to my mom in case she has to go to the store.
Look at the rating on the filters. I’d guess it’s something like FFP3 or N100, which means better than N95.
Would failure to rigorously follow CDC recommendations be a basis for a legal case?
For whom against whom?
Anyone against anyone else. They’re suggesting that maybe the cdc is avoiding recommending face masks because e.g. then grocery stores that don’t provide them to cashier’s are disobeying Official Recommendations and could be held liable.
I have no idea if this was a consideration, but I think any civil claim can in principle be resolved by a jury and I imagine some jurors would find the cdc recommendation meaningful.
Two thoughts on the topic.
First, separate from whether they reduce your chance of getting infected, are surgical masks a good idea because broader use would stop people who are infected but think they are healthy from spreading the virus prior to being symptomatic. This harnesses people’s desire to not get infected for the purpose of reducing their risk of infecting others. To some extent it seems like a guideline that treats your infection status as known is less useful than one that incorporates the uncertainty.
Second, in the experimental design for a mask effectiveness study, could you overcome the intention-to-treat vs per-protocol conundrum by asking some families to wear actual surgical masks and others to wear known-to-be-ineffective masks (or some other placebo that requires compliance). Then you could remove the non-compliant from both groups, hopefully controlling for general diligence, and get a read on the effectiveness of the real masks.
I think the CDC is also very worried about people risk compensating. We already have a big problem with people who are being told to quarantine going out to huge parties instead. If the CDC came out and said that masks were even mildly effective there would be a massive rush of idiots going and either buying up the few remaining boxes of making their own, then going about their day like usual because they think themselves invincible. By telling people they aren’t effective then yes a small number of people who would have been saved by wearing a mask will get infected, but overall it is probably keeping more people indoors which outweighs that cost.
I have my suspicions that this is their reason for the recommendation not to wear masks, and I’m somewhat surprised Scott didn’t bring it up (considering he mentioned risk compensation essentially one paragraph after wondering what reason the CDC could have for its recommendation). Of course the CDC would never make this reasoning known to the public – at least while the pandemic is still a serious public health concern – since that would destroy the effectiveness of the message.
I also think Scott is right to say that using a mask could be a harm even if you risk-compensate just a little bit. It wouldn’t just be people who tie a bandanna around their mouth and go to a party. I have personally been avoiding the temptation to use a mask in public – even though my workplace has a small supply of N95 respirators (used here to filter caustic dust; I’m not in healthcare) – because I don’t trust myself not to use the mask as an excuse to take on unneeded risks like stopping at the supermarket a couple extra times a week. Risk compensation can be largely unconscious, and can happen even if you understand how it works and are fairly careful.
I love this
Can you elaborate on the “failure” rate of an improperly fitting n-95 mask vs a surgical mask? It seems like even if there is some small leakage on the n-95 (“failure”), it will be a lot more close-fitting and still work significantly better than a surgical mask. I’d think that in reality it’s more of a continuum rather than a binary pass/fail analysis of its function that matters, which is especially relevant since you point out that the amount of virus you take in is probably important. (Edit: e.g. if you imagine wearing one for working in a dusty environment, wouldn’t you just want to wear whichever blocks as much dust as possible, even if a little still gets through? It is a little different from something like scuba diving gear wear any leakage is unacceptable because it means your facemask fills with water so it’s essentially pointless?)
Not an expert, just speculating. I think it boils down to two effects:
1. If 10% of air doesn’t go through the mask, it’s much less relevant if the rest has 99% or 95% filtration – you still end up with a 10x reduction instead of 100x
2. Surgical masks being softer might help form an ad-hoc seal when you inspire – they tend to follow the form of the face. N95 are more rigid, if they don’t fit that’s it.
Also being less filtery might perversely help with the seal – less negative pressure.
I was expecting “failure” meant that it wasn’t perfectly sealed so some amount was not going through the mask you seem to be contemplating that what is going through the mask isn’t filtered properly, and either could be an issue but I thought they meant the first type of failure, given the emphasis on the proper fit. So I would imaging a failure like that to mean that a very small amount of the air leaks in, more like 1% or something rather than 10%.
But this makes me think that it is just too extreme to act like these massive reductions aren’t important.
Otherwise, why not say that the Lysol wipes or hand sanitizers that kill 99.99% of germs are a complete waste of time because anything less than 100% is a failure which apparently doesn’t help?
Some have mentioned a side benefit that we should take seriously: the sight of people wearing in public is striking and unmissable.
Under present circumstances, it’s a billboard that says “I am taking social distancing seriously, please don’t come near me”
It also might help win over the chimp brains of anybody who’s not yet staying at home/distancing. When everyone else is on team mask, and you get weird looks at the park, it hits in a visceral way that “government press release” might not.
In my experience, the only thing that wearing a facemask in public means is “I am East Asian”.
I remember one time back when the wildfires got really bad, one of my Chinese coworkers handed out masks at the office. I didn’t bother trying to figure out how to wear it.
I saw a white person wearing a mask for the first time the other day (Oxford, UK).
He appeared to be out for a walk with his East Asian girlfriend.
+1. When I went to the supermarket here in Portugal, and saw the staff wearing masks, it really was a shock and made me automatically more conscious and adjust my distance regarding the other customers.
PS: Here in Portugal they also recommend against the public wearing the mask. (They probably take their cues from the US.) I wish that would change because of how overcrowded public transportation is.
As a fan of Harbor Freight (a US nationwide store selling mostly low-priced Chinese imported tools), I was pleased to see that they had decided to donate their inventory of N95 masks, face shields, and nitrile gloves to hospitals in need. The announcement gives details on how obtain vouchers: : https://www.thedrive.com/news/32698/harbor-freight-to-donate-entire-supply-of-masks-gloves-to-hospitals-nationwide.
I too am a fan, and more so now! Thanks for sharing.
this study (https://pubmed.ncbi.nlm.nih.gov/30229968/) seems to be making the rounds on twitter as evidence that experts are bullshitters as much as that masks work. but only the link only shows the abstract, not their model. has anyone who has read this study comment on their model?
Full text: https://sci-hub.tw/10.1111/risa.13181
Having just skimmed the paper it seems like the paper is assuming masks decrease transmission rates involving the wearers (either less likely to get infected or less likely to spread, I didn’t read close enough to distinguish) and then do mathematical modeling to show how that would impact an epidemic. So it’s more about “if masks are effective that helps society” than about proving masks actually are effective.
I didn’t read it that closely, but it’s a modeling paper. A modeling paper doesn’t seem like it would make sense to prove masks actually influence transmission rates or not.
I find that many people come to a conclusion on a complex issue, then reduce it to a Rule. The tendency to remember the Rule and forget the evidence and reasoning that supported that conclusion. The Rule acquires the same moral force as the end it is meant to promote. Because they have forgotten the original reasoning, they are resistant to new evidence. They cannot weigh new evidence against the evidence supporting the original conclusion, so that new evidence goes unprocessed. They stick to the Rule, and often resent and mistrust a person challenging the Rule. Highly conscientious people seem particularly prone to this.
The process is cognitively efficient and well suited to an environment in long term stasis, as human society had been up until a couple hundred years ago. Bureaucrats tend to be in the rule-making business, and are prone to this reduce-it-to-a-Rule mindset. A fast-changing crisis situation can force them to recover that old evidence and reprocess with new evidence or a new context, but it just happens slowly.
+1 to this. Don’t know if it’s original to you or not, but it explains a lot.
That’s one of the reasons I think the crisis will do good as well. Lots of Rules are suspended while it lasts, and when it ends… some people will slip back in, but some will start thinking.
Scott Greenfield (https://blog.simplejustice.us) calls that “remembering the rubric while forgetting the rationale”. He’s not as positive on it as you are, but then he’s a legal curmudgeon.
Actually figuring out what to do from first principles in most situations is way, way too slow and error prone even for those who are good at it. Imagine, say, negotiating road traffic by constantly thinking hard.
Can we all wear scarves over our faces? I fee like there’s enough fabric for that.
This is just mind boggling. Home Depot and Lowes sell god only knows how many P100 respirators all year to painters, so they don’t huff paint VOCs all day long. They work, and don’t as near as I can tell, require any training. Certainly mine makes a world of difference. However small viruses are, VOCs are even smaller.
I’m pretty sure OSHA says painters have got to wear these things. Have OSHA and the CDC gotten together to reconcile their advice, taking into consideration the relative mass of the particles they’re concerned about blocking?
Rubber respirators are easier to fit. N95 have somewhat tougher edges.
But the one-way valve on the P100 respirators means that you are better protected from the outside (you get a better fit), but the outside is not as well protected from you (you exhale out the valve). I wonder if they could just put a surgical mask style cover over the outlet from the valve to filter some of the badness out of the exhaled breath, too.
Good point.
Just tossing this up on here during a brief break from work: Somebody’s marshaling of a few studies to make the case that masks make a substantial difference, and surgical masks nearly as much as respirators.
https://smartairfilters.com/en/blog/n95-mask-surgical-prevent-transmission-coronavirus/?rel=1
I know, I know, site is an air purifier company. But my quick impression of the company and of the studies they cite was that neither can just be written off.
Hope some folks here will give the several studies cited on site a look and post your take on this stuff. I will too, end of work day.
This short Twitter thread agrees: “Public should know covid exposure dose matters. We have to conserve masks for healthcare workers, but masks can help anyone, reducing amount of virus released (even by breathing) or taken in. Immune system is more effective if infection starts w/ low dose.” https://twitter.com/PeterKolchinsky/status/1239560638239838215
It’s from a biotech investor, but he has a PhD in virology, and in the replies he cites this study which he says demonstrates “correlation of flu dose with severity of subsequent infection in mice”: https://pubmed.ncbi.nlm.nih.gov/16356862/
Yeah I saw that too. Made me wonder about the idea of doing a very crude version of immunization by giving people a very tiny dose of live virus. Might be worth it, if subject develops immunity with greatly reduced chance of developing severe illness. Have no depth of knowledge in virology, etc., just brainstorming here. Wonder if any groups of researchers are looking into an idea like this. Anyone know?
They used to do this with smallpox–it was called variolation. You usually didn’t get as sick a a normal case of smallpox, but sometimes you got full-blown smallpox and died.
I don’t understand why no one is mentioning using a furnace filter as a DIY material for masks. I bought a MERV 16 rated filter of size 16x25x4. From that I stripped off the cardboard frame and the foil mesh and was able to make about 75 filters of size 7″x4″ (same size as a surgical mask). MERV 16 is rated to stop 95% or better of particles between .3 and 3 microns of size. If you can’t find a MERV 16 rated filter, you can use lower rated filters like MERV 13 or 14 which should also help.
After I cut the filter into 7″ x 4″ strips, I reinforced the sides with a small square of tape and used a hole puncher to punch a hole on each side. Through each hole, I passed a thin elastic cord of about 9.5″ and tied it into a loop (for the ear loops).
At the top of the mask, I created a formable nose clip to block out air, since that is where most of the air leakage will come from. I took 20 gauge solid copper wire and cut 2 strips of about 3.5 inches long. I then taped those two wires horizontally to the top of the mask. The wire is malleable, but slightly stiff. I used 20 gauge because that is what I had at home, but a thicker gauge would work and would not require 2 wires for the proper stiffness. (Anything that is somewhat stiff but also formable would also work.)
I did one last thing. The upper corners of the mask were bothering my eyes so I cut a small diagonal strip off those corners. And there you have it. One thing to be aware of is that direction of the fabric does matter. When you first get the furnace filter there will be a wire mesh on one side. That is the side that should be touching your face.
When I put a bottle of vinegar to my face, I could still smell it with the mask on although the odor was much reduced. When I put an N95 mask on, I could barely smell the vinegar.
If you have any dust masks at home, an easier way to make a mask might be to take the furnace filter paper and use it to line the inside of the mask. I haven’t tried that yet.
Majorly over-simplifying, but it occurred to me that the absolute minimum standard for a face mask to be worth wearing is probably “better than coughing into your elbow.” Are there any masks which don’t meet this standard?
This was my thought as well, though I can believe that’s also barely effective. Maybe coughing into the elbow is mainly just intended to displace a natural behavior of coughing into the hand, in which case it would help by keeping people’s hands cleaner even it barely controls the respiratory ‘overspray’ at all.
> After the pandemic is over, scientists look at the health care workers who did vs. didn’t get infected, and see whether the infected people were less likely to wear masks
There are trials outside of medical settings, e.g. this metareview of mask usage during mass gatherings and this one in schoolchildren
Startup idea: have people scan their face with their phone and 3D print N95 masks to best fit the scans. Even if we don’t get it started in time for this epidemic, we can be ready for the next. Or is someone already doing this? (I know some companies are doing this for headphones).
The basic idea has already been done, and there’s a pdf giving the basics of how to do it. https://www.thingiverse.com/thing:4167649
The problem is that it’s not at all straight forward as it stands.
thingiverse.com seems to be broken at the moment and I can’t access the pdf. Is the scanning the problem? Labs could use Kinects..
I recently co-authored a scientific commentary on this:
“Promoting simple do-it-yourself masks: an urgent intervention for COVID-19 mitigation” (Svara et al., 2020)
Preprint: https://link.medium.com/LY7RRNr2X4
Basically, we argue that even simple DIY solutions such as cotton/T-shirt cloth can reduce spread of droplets (and derived aerosols) BY THE WEARER, and should therefore be publicly promoted (or even enforced) until medical grade masks become available.
The focus should be on broad adoption and reduction of released droplets, not protection of the mask wearer.
I think you misinterpreted the studies on surgeons performing surgery. Those studies are assessing the risk to the surgery patient, not the risk to the surgeon. A surgeon operating on a patient who has COVID-19 definitely needs an N95 mask, because they’ll be exposed to a lot of infected bodily fluids and many surgical procedures will generate aerosol.
Might not the really useful part of mask-wearing be the part where it protects others from you? In that case, what we really should have done is produce gigantic piles of masks, and then have the CDC bend the evidence the other way to get everyone to wear them.
Since we don’t have enough as it is, not useful advice for the moment. BUT, if the possibility of a summer lull and an autumn “second wave” is real (as happened with Spanish Flu), then we should really consider having this set-up. In this way, I think, the current CDC recommendations are extremely harmful: they can’t easily reverse their ruling without smashing their credibility into atoms.
PS: Update on the whole “traveling across the country” thing from the recent Open Thread (for anybody interested). Thanks to everyone who gave me advice! As recommended, we drove and slept in hotels, and we made it to the West Coast in a total of 4 days without much trouble. Simple safety precautions: gloves for any activity which required touching things outside our car or hotel room; masks for any situation where we had to be indoors with other people; lots of hand sanitizer and wipes; pre-paid tolls to save time and reduce the need to get close to people and/or handle cash; lots of food packed to avoid needing to buy it along the way. Traffic seemed sparse, even near large cities, and very little human contact was needed (we only talked to a few hotel clerks and one or two gas station cashiers).
Of course, we won’t know for a few days whether we successfully avoided infection, but everything seems good for now. So thanks again to everyone.
FDA is now banning at-home SARS-CoV-2 test kits… are they actually TRYING to Kill All Humans, or does something in the FDA building air system lower IQs?
https://techcrunch.com/2020/03/23/updated-fda-covid-19-testing-guidelines-specifically-disallows-at-home-sample-colllection/
In a just world, everyone on the FDA chain of command for test approvals would be in prison or executed for negligent homicide.
Don’t hate the player, hate the game. The FDA is behaving according to its institutional mandates and its internal culture and incentives. If we want different behavior, we need to change those things.
I never understood why we shouldn’t hate the player in addition to hating the game.
“Overriding your incentives for moral reasons” should be a part of what it means to be human. Additionally, that becomes part of the ‘game’, so long as we can hate (and punish) the players too.
I predict that it will be easy to morally condemn the FDA people, but that if we don’t alter the mandate/culture/incentives of the FDA employees we’ll still get the same pattern of behavior. Not exactly the same, of course–the clusterf-cks in the COVID-19 response and a desire not to screw up in that way again will probably become part of the FDA’s culture. But they’ll behave according to their incentives/mandate/culture, so we should look to change those things if we don’t want the same kind of behavior.
Alternatively: knowingly being part of an immoral system makes you an immoral agent as well.
I think this is too simple, and indicative that you might have minimal contact with GS10+ people generally, or have had a non-representative experience.
The FDA culture is representative of GS culture. I’ve been an intern working at agencies, worked full time, and currently work with/against them on a regular basis. The only way to change it would be to change hiring policies and go back to an old school spoils system, or something like it, for millions of employees. Its a stable, high-mid paying job that only accepts high qualified (academic) applicants. What this means is that actual high level independent minded people quickly leave via being hired for 2x+ salary or are fired for rocking the boat. Often they are fired from the bottom up. The most talented coworker I had at an agency was reported multiple times by people at or slightly below her GS level. She was not retained. The least talented one I know was a reporter, he was retained. He still works there. The only good superior I had there was a quiet guy who followed all the rules and had a sick kid so he couldn’t risk private sector health insurance.
Its a product of civil service (teaching has the same issue), not the FDA. And the problem isn’t superiors, its that employment is for cause firing after an initial period. The sources of the problem predate the FDA by almost a century.
> The FDA is behaving according to its institutional mandates and its internal culture and incentives.
Isn’t this akin to the whole “deep state” model, only in what would usually be a boring and apolitical organization?
I think it’s the same idea as the deep state, if you use that term to think about how things work rather than as a tribal identifier. Agencies have a culture. I think FDA’s culture is a mix of science and caution.
Without knowing the quality of the tests or risks associated with random people trying to mail bio-hazardous materials, it’s really hard to say how bad of an idea this is.
Ceterum censeo FDA esse delendam. Too bad, I wanted one of the antibody kits, as I’ve quite possibly been exposed; it’s not really of any practical use to me to know if I had a mild or asymptomatic case, but I was curious.
It’s was kind of funny to me for a second to hear that someone who’s been through medical school has “a vague sense” that one virus isn’t enough to infect someone, but it makes sense, probably almost no one actually has any informed idea about this. How do you create a study where the outcome is infecting people with a disease? (In a way that is ethical, the unethical version is trivial.)
Actually, as I was typing that I was reminded of some of insanely unethical experiments I’ve heard of done by e.g. the Japanese during WWII, and of course others; I don’t know much about them, and what I mainly remember is experiments designed to observe the progression of a disease. But perhaps that body of work would be a place to find some results on this subject. I imagine that a government which is developing bioweapons would be very interested in how infection chance scales with delivery of viral particles.
They do studies like this from time to time. I remember hearing on TWIV about some studies like this done for norovirus. (Amazingly, they can get people to voluntarily be swabbed with norovirus for a couple hundred bucks. This is a fluids-coming-out-every-opening kind of bug that makes you genuinely miserable for a couple days–they’d have to pay me a *pile* of money!).
If I understand correctly (please someone correct me) they first figure out how many infectious particles they have by doing a plaque assay (swabbing onto a cell culture plate with cells vulnerable to the virus, and waiting to see if some cells on the plate start dying), and then doing successive dilutions to get down to the point where they regularly stop getting any dead cells. Then they know what concentration to use to give you approximately N infectious particles.
IIRC, norovirus was something like 10 infectious particles to get sick. (A quick web search said <100 infectious particles.) That plus it being a very robust virus (protein coat, no bilipid membrane, not particularly sensitive to alcohol sanitizers) is what makes it spread so well. Fortunately, coronaviruses are much less robust, since they're enveloped (they have a bilipid layer that can be disrupted by soap or alcohol, and then they no longer are infectious).
Wikipedia article on plaque assays and virus quantification experiments.
Why is it unethical to infect people with mild diseases? I’d gladly participate in a study where I get infected with one of the common cold coronaviruses in exchange for $200, especially if I thought the study had important public health implications that could one day protect me from a pandemic. If you want to infect me with influenza, maybe $1000.
When I was in 6th grade, I made a remark to my mother about how ridiculous the verdict in the OJ Simpson criminal case was. My mother correctly chastised me for my remark. One reason was that I had not reviewed all of the evidence the jury did, I did not review the evidence as in depth as the jury did, and I wasn’t present for the jury’s deliberations. I should instead trust the decisions of those who know more about the case then I do. This is an important point but not what this rant is about.
The other reason is that the jury finding of “not guilty,” is different then a jury finding of “innocent.” The jury stating that it couldn’t conclude that the accused was guilty does not mean that the jury concluded that the accused was innocent. “Not guilty,” more properly means “not determined to be guilty” and not “determined to be not guilty.”
I tried making this point to my father when he made an offhand remark about the ridiculousness of the verdict. He found this distinction to be absurd (a person is either guilty or he’s inocent so if he’s not guilty that must mean that he’s innocent) and made it clear that he wouldn’t entertain any consideration that there could be a third category. Both my mother’s reaction and my father’s reaction made an impact on me.
Over the years, I have developed a more sophisticated understanding of this dynamic and I’ve come to the conclusion that people are frightened by their own ignorance. I have seen similar reactions in a wide range of different situations.
I have often come across somebody stating “____ doesn’t make sense,” whereas instead they should be saying “I don’t understand why ____ makes sense.” Everything that can be observed has a reason for it though it might not be a good reason. Not knowing why something makes sense just means that one is not in a position to evaluate whether the reason is a good one or a bad one. However it is more common for people to conclude that because they personally are ignorant of the reason for it, such a reason must not exist (or if it does, it must be a bad one).
I remember once stating a fact from physics to my uncle (as background, I have a BS in physics, my uncle has a BA in sculpture) and remarking that I can’t remember why the fact is true (or why I came to that conclusion: I can’t remember the specifics). I did offer to come up with some BS reason that sounds like makes sense but would almost certainly be wrong because I would just be making it up on the spot from whatever happened to come to mind first. He asked me to do so and I came up with exactly that. He believed my explanation because it made sense to him (even though he had absolutely no ability to analyze the explanation I gave and I encouraged him not to believe it).
I have often challenged a conclusion someone has come to (in the sense that the other person hasn’t demonstrated the voracity of their conclusion enough for me to believe it) only to have them ask me for why they should believe that the conclusion is false. The thought that I would be agnostic on that particular conclusion doesn’t even appear to be a possibility.
I could go on but I have found ample evidence that people have a tendency to confuse their ignorance for knowledge. The inability to distinguish “no evidence for” from “there is evidence against” seams to be universal (or nearly so) in humans: not just doctors (who, weirdly, seam to have problems recognizing that they’re human).
For my part, I tend to estimate that somebody stating their ignorance to be more knowledgeable then someone who acts like they have none. Recognizing and admitting ignorance is a statement of strength whereas pretending like one doesn’t have any is an admission weakness. I figure that this is the opposite of people’s visceral reactions. I believe that it is this dynamic that explains this particular epistemological failure.
Did you ever learn?
When fires came to the Bay Area, did you still have the skill? Did your local friends learn it? Does a poorly worn face mask provide some comfort against the bad air? (If not, then your friends probably got a lot of practice and did learn it.)
I’m looking for good data about persistence on surfaces. As background, most of what I’ve read suggests that COVID-19 is probably spreading mostly by droplets. You cough and spread a gazillion disgusting little droplets of water, mucus, and virus particles in a cloud in front of you, the droplets land on the doorknob, I open the door and rub my eyes, and two weeks later, I’m hitting the local hospital up for an ICU bed. Knowing how long those droplets’ payload of virus particles is infectious seems really useful for knowing how to respond.
What I have seen so far is:
This experiment from 2015 with a human coronavirus that causes colds looked like about a 100-fold reduction in infectious particles in four days (how long the experiment ran).
This NEJM paper linked from TWIV tested SARS and COVID-19 for persistence on surfaces directly–it looked like on all surfaces, they were down below detection limits after three days, with a half-life around 7-8 hours for plastic and shorter for other surfaces.
This survey paper collected estimates from many different sources, and said that virus particles might survive as long as 9 days on some surfaces.. But it looked to me like there was really wide variation between reported numbers even for the same virus from different papers, so I don’t know what to make of this–probably this comes down to different experimental setups or something.
There was also this WHO report from early in the SARS outbreak, cheerfully describing how long SARS virus persists in urine and stool.
Finally, this note from the CDC said that viral RNA remained on surfaces of the Diamond Princess (the cruise ship that held all those quarantined sick people in a Japanese harbor) 17 days after exposure. Note that detecting RNA doesn’t mean the particles are infectious, though. Coronavirus is enveloped, and once the envelope degrades, it’s no longer infectious, but the viral RNA is still around. OTOH, it doesn’t look like they did any experiments to see whether they could get infectious particles from sampled surfaces on the cruise ship, so we don’t really know.
The stuff I read generaly said that common disinfectants do a good job killing the virus off, though I wonder whether the lab conditions are very close to how they’re actually used. (What fraction of virus is killed by a halfhearted swipe of an almost-dry Chlorox wipe on a doorknob by a bored janitor?) And a bunch of these papers pointed out that on copper surfaces, the virus doesn’t persist long at all. (At this point, I’m for replacing all high-touch surfaces in hospitals, homes, offices, and public places with copper/brass/bronze. See, that’s where our stimulus dollars should go–to coating the world in a layer of copper!).
Also, this PDF file shows recipes for making disinfecting and santizing solutions with water and bleach. (Sanitizing solution is stuff you can use in the kitchen on surfaces that will have food on them later, without rinsing. Disinfecting solution is what you use on the bathroom tiles when your kid pukes on them).
As always, I’m an interested amateur, so if someone knows more, please correct me.
As an addendum, it’s maybe useful to think in terms of half-life of active virus. If half-life is 8 hours, then every day, you get about a factor of 8 loss of active virus–after three days, the number of active viruses has fallen by a factor of about 500. if the half life is four hours, then things are better–every day, you get 1/64 of the viruses you had before; after three days, you’ve got about 1/250000 of the viruses you started with.
I’m not sure how well reality tracks with the half-life model, but this kind of gives some intuition for me thinking about the problem. If I make a naive linear model of probability of infection given viral dose (ignoring multiplicity of infection), then every half-life I leave a potentially-contaminated surface untouched at room temperature conditions, the probability I’ll catch the infection by being exposed to that surface gets half as big.
I haven’t found a discussion to the article “Physical interventions to interrupt or reduce the spread of respiratory viruses”, from 2011, a Cochrane review (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6993921/).
It comes out generally in favor of wearing masks. What do people think?
What I didn’t see mentioned in this writeup is that practically any mask could still reduce the viral load in case of exposure – even if you get hit by airborne particles through the mask, some of their volume will get stuck on fibers of the mask instead of making it into your respiratory pathways and your immune system might have a slightly easier time of mounting a response.
I guess I’m wondering why the null hypothesis has to be “masks don’t work” and that’s the default action until poven otherwise? It seems reasonable to assume the effect is >0%. So – shortages notwithstanding – why wait for a study to tell you to wear one rather than the other way around? Isn’t a Type I error when dealing with infectious diseases preferred to a Type II error?
2 main reasons:
First, the technical or engineering claims. When an engineering or technical claim is made, there’s a set of professional and legal consequences that go along with that. If someone sells bolts rated for 500lbs and they don’t support 500lbs, the seller might be on the hook not just for replacement but also costs all the way down the line. The manufacturer would hate to discover they were key elements in a skyscraper or something. But the reverse is also true. Somebody designing something is able to rely on the claims of other professionals. So assuming a Design Professional decided that a 500 lbs bolt was appropriate for a particular application and specified such, the fact that the bolts were defective and thus the skyscraper fell over and killed a bunch of people would not come back on them. (If you want a detailed write-up, you can probably badger CatCube at some point)
We know that you have to get virus into you to get infected. Surgical masks are not designed to keep viruses out. They certainly aren’t manufactured according to a process designed to ensure that the final product will keep viruses out. So that manufacturer doesn’t claim that they keep viruses out. So therefore they “don’t work” because nobody who risks any legal responsibility for being wrong is claiming that they work.
Second, what does it mean to say that “it works”? As noted, even the N95 masks don’t claim 100% perfection. They do make specific claims about reductions when used appropriately for certain types of particles. This is an engineering claim of performance. Then, separate panels of experts at organizations with names like FDA, CDC, NIOSH, etc. conclude that such a standard sufficiently reduces the risk of exposure or infection so as to be “safe” for workers in those fields. That is, they “work” to mitigate the hazards. Or at least avoid an OSHA violation. But surgical masks aren’t said by any regulatory body to “work” for anything that I know of.
Ultimately, since this is potentially life-threatening, no professional is going to want to recommend something in any manner which might be interpreted as “this makes you safe”. To do so violates ethical norms and potentially puts them on the hook for various types of liability.
Engineering example makes sense. I hadn’t thought about it through the lens of a medical professional.
The cost of wearing a mask is not zero: they’re uncomfortable and annoying, and there is effort involved in acquiring or producing them. So the expected benefits of wearing one need to be significant, not just probably non-zero.
Scott, this is a great article, however the shortage problem is really a non-issue as proven by the Czech Republic. They’ve mandated that the entire country starts wearing masks starting from March 19th, even though there’s a huge mask shortage there as well. But if there aren’t masks in pharmacies, what do you do? The Czech answer is to simply have everyone make a homemade mask:
1. People can wear a ski mask or a bandana or a scarf, as long as it covers their nose and mouth
2. You can make a simple disposable mask out of a paper towel and two rubber bands
3. People who own a sewing machine started making masks from textile and distributed them to the public free of charge (check Damerousky.cz for a map of free mask distributors)
As a result, everyone wears a mask now in Czech Republic. Those who don’t get fined by the police. The vast majority currently wears a homemade mask to ensure that healthcare workers get the professional ones. What stops other countries from using the same approach?
Mandating the wearing of masks is a great of flipping the switch from “it’s weird to wear a mask” to “it’s weird to not wear a mask.”
In low-risk situations, like being at home or taking a walk, I mean sure, a mask might make you 0.0001% (or whatever) less likely to get infected. If that’s worth it to you, consider the possibility that you might be freaking out a little too much about this whole pandemic thing. If it’s still worth it, go for it.
The Massachusetts Audubon Society has closed all its parks because lots of people were hiking the trails and they considered that unsafe. A requirement to wear a mask on the trails would seem to be a better alternative.
I think the evidence that a) masks help, and b) that everyone has something they can stick something in front of their face is strong enough to promote makeshift mask wearing right now.
As has been mentioned above, in the Czech Republic people were able to go from 10% wearing a mask to 100% in the space of 4 days (this number from contacts in the country). Supply for the general public can be worked out astonishingly rapidly via makeshift homemade masks.
Secondly, while it is true that mask wearing, if it does anything, reduces your chance of infection from an already very low number (“0.0001% or whatever”) to an even lower number, the game that decision makers are trying to play right now is to reduce the infection risk of everyone in the country from a low number to an even lower number. I don’t fully understand why the decision problem looks different from an individual and a collective point of view, but staying at home reduces your infection risk from a low number to an even lower number, and everyone is recommending this right now (including me!)
Thirdly, there are a couple of weak studies that do try to investigate the impact of mask wearing by the general public. They also do this for SARS, which as far as I understand is the best comparison we have for COVID (otherwise known as “SARS 2.0”). They both find large effect sizes (odds ratios of around 0.3), but I think these are overwhelmingly likely to be overestimates given weak study designs.
Lau 2004: https://wwwnc.cdc.gov/eid/article/10/4/03-0628_article
“he univariate analysis were used as input for the multivariate stepwise conditional logistic regression analysis, the results show that among the 330 patients with undefined sources, the following were significant risk factors: having visited mainland China (OR = 1.95, p = 0.020, Table 2), having visited the Amoy Gardens (OR = 7.63, p < 0.001), having visited the Prince of Wales Hospital (OR = 7.07, p = 0.009), and having visited other hospitals or clinics (OR = 3.70, p < 0.001) during the reference period. On the other hand, using a mask frequently in public places (OR = 0.27, p 10 times a day (OR = 0.58, p = 0.008), and disinfecting the living quarters thoroughly (OR = 0.41, p < 0.001) during the reference period were significant protective factors (Table 2)."
I think this mainly shows that being paranoid helps, but it’s not clear how best to be paranoid.
A similar conclusion is reached in Wu 2004 (https://wwwnc.cdc.gov/eid/article/10/2/03-0730_article): People who didn't get SARS did lots of sensible things cases didn't, including wearing masks.
It’s possible that the mask-wearing mandate is safety-theater, much as the TSA is security-theater. It looks like something is being done while not having a significant impact on actual safety or disease communication. This is worse if people then compensate and proceed to engage in activities they otherwise wouldn’t if they didn’t have the false sense of safety of wearing a mask.
We don’t know how well the home-made masks are going to perform, either in terms of disease transmission or acquisition. Hopefully well. But I don’t think we know yet.
So, in spite of the evidence that they are effective, they might not be. True, but an odd position to emphasise.
Do you think people will risk compensate away all the gains and then some? Even if 100% of the benefit is risk compensated away, there is still a benefit because people are now living freer lives at the same level of risk (this is true even if it’s *slightly* more than 100% of the benefit).
Given that we don’t have time to do a detailed study into the efficacy of homemade masks now, do you think that the best judgement given what we know is not to wear them?
I think the case for wearing them is very strong.
This might be a really dumb question.
Colorado just reported that the 165,000 masks they got from the Strategic National Stockpile will last for one day.
I assume this is because the standard for healthcare professionals is to change PPE for every patient and activity. Otherwise the mask itself may be carrying disease from patient to patient. So if you want to test N people for coronavirus, there go N masks. If you want to check N patients’ vital signs, there go N masks. (Presumably you could change this procedure in a hospital containing nothing but confirmed coronavirus patients, where you are basically just trying to protect the doctors and nurses, but that sort of change seems like the kind of thing our society struggles to do.)
If that’s right, is it completely obvious that this is the highest use of scarce masks in a pandemic? There are a bit less than 5.8M people in Colorado, so roughly speaking you can either equip healthcare workers in the state with (dozens? hundreds?) of masks per day or you can give every man, woman, and child one mask per month to (re-)use for weekly trips to the grocery store or whatever. If the latter bent R down a bit, wouldn’t the formidable asymptotics of (decreased) exponential growth soon dominate the merely constant difference between the exposure of healthcare workers and the exposure of the average person?
Among the many ways this could be wrong:
(1) Actually 28 masks per day per 1,000 population represents much more careful conservation of masks by the healthcare industry than I think. Decreasing this number by an order of magnitude would result in every healthcare worker getting sick, or drastically increased spread of the virus in the healthcare setting
(2) Reusing disposable masks for a few trips completely defeats their effectiveness for some reason that’s not obvious to me
(3) Masks in ordinary people’s hands are so useless that they can’t decrease the growth rate of the epidemic even slightly
A virology blog post about aerosol transmission. It was originally written talking about Ebola, but it has a figure that has been updated to talk about infectious droplet sizes from COVID-19.
ETA: The FDA is allowing experimential use of COVID19 survivors’ antibodies (spun out from their blood) as an attempted treatment for very sick patients. Anyone know much about this? I’ve heard of it, but don’t know how likely it is to work or whether it’s likely to cause other problems. (The article talks about antibody-dependent enhancement of infection as a risk, but I think that’s a super-rare thing that’s only really known to happen with Dengue.)
It happened with one flu strain in 2008-09 also. And more relevantly, original SARS.
Gamma globulin shots of antibodies were somewhat-regularly given to schoolchildren in the 60’s; my mom got them.
I got them as a kid, too.
I think they did the antibody extraction trick for Ebola as well. It’s basically the lowest-throughput highest-cost treatment of theoretical efficacy available, used only when nothing else is available.
I presently do wear a mask in these situations, and I wear a powered, air-purifying respirator (PAPR) in higher risk ones. But that is only because I am working on a subunit vaccine that I intend to test on myself, and it is imperative that I not be infected before then (a week or two, and a couple weeks after that to measure antibody production). There is plenty of work being done on killed and live attenuated vaccines, but those take longer to scale ( although have a greater likelihood of working well). I have very low confidence in dna or rna vaccines, but would be thrilled to be proven wrong as those also have the potential to scale rapidly.
The ghost of John Scott Haldane smiles on your endeavors.
One important aspect of wearing any kind of face mask is that it prevents you from touching your face.
I am pretty sure it would lead to me touching my face more due to discomfort/irritation.
I don’t know how trustworthy this is – but this presentation https://drive.google.com/file/d/14tGJF9tdv4osPhY1-fswLcSlWZJ9zx45/view?fbclid=IwAR0qDDOK5dzri10VSjN5caExycAVScfOpsZcC19_uaZxsBG-W-jJMOd5XS0 claims that none of the 42000 health care workers that were brought to Wuhan from other provinces to work with COVID-19 patients has caught COVID-19, and that was because of using the proper protection. The photos show full body protection with surgical masks not respirators. This could be a relevant data point if it was true.
Maybe it’s true, but why would you trust anything China publishes?
You can forgive the CDC of some weird institutional language wonkery and the resulting public confusion, but can you say the same for the Surgeon General?
https://twitter.com/Surgeon_General/status/1233725785283932160
This is certainly my dad’s opinion, who used to inspect health and safety in hospitals. During a recent discussion about masks and COVID-19, he said dismissively “nobody in a hospital has a clue about proper mask use”.
Just as an aside, you and your father may think this is a statement about the ineptitude/indifference/bad training of doctors, but actually, it’s a strong indication that current disposable N95 masks suck. This is safety equipment that is routinely misused by professionals who use it every single day, even when they know they are in a high-threat environment where the safety equipment might save their life.
One thing we should get out of this crisis is masks to protect against inhaled airborne droplets that actually are usable by nearly everyone who gets some decent level of training on them.
P100 respirators (other names outside the US) are designed to protect their wearers from similarly small particles, and seem to me to be much easier to use correctly. They are, in fact, routinely used by do-it-yourself-ers for home projects, and Californians during fire season. The two I have (bought from Home Depot–nothing special) have rubber seals that press against your face and straps that hold them on. They seem not to be especially hard to use. The problem is, they have a springloaded one-way valve. When you exhale, the pressure opens the valve and lets your breath out; when you inhale, the valve is closed and the air comes in through the filter cartridges. That seems to do a lot better at protecting you from the outside, but doesn’t do a thing to protect the outside from you.
Here is my proposed quickie design. (Supplies for hand building this are unattainable right now.).
a. Start with a P100 mask of this kind, which seems to be much easier to fit and use, and which is routinely used with apparent success by lots of novices.
b. Make a “beak” of filter medium from a disposable N95 mask.
c. Use duct tape to seal the filter medium beak around the outlet valve. (In a final design, this would be the disposable part of the mask that was routinely changed.)
On the inhale, air goes in via the cartridges. On the exhale, it goes out through the valve, and then through the filter medium “beak”. The work of exhaling is increased, but it depends on the surface area of the beak, and we can make the beak bigger to decrease the work.
The seal against the user’s face is done with a rubber seal that’s much bigger and more flexible and better in basically every way than the disposable mask seal. The seal of the filter medium is done against a flat plastic shape with tape or some kind of dedicated, designed seal.
When you cough or sneeze inside the mask, it comes out the output valve and goes through the filter medium before reaching the outside world, protecting those around you. When someone else has coughed airborne droplets into the air, you inhale through the filter cartridges and are protected. The “beak” will eventually collect too much moisture and become less effective, so it needs to be changed out from time to time, but it will always be doing at least what a surgery mask does–catching the big droplets.
You can clean everything but the filter cartridges/medium with normal sterilizing wipes or whatever.
Second proposed quickie design:
We start with a permanent mask that’s got the straps and rubber seals and output valve, but without the filter cartridges. We use duct tape to create a good seal over all the openings (including the openings where the cartridges would normally go). The permanent part of the mask is fitted to you and the permanent rubber seal is against your face. The seal between the disposable filter medium and the permanent mask is done with tape or some other mechanism, but it’s easy because it’s against a regular surface and can be taped or tightened down without hurting the user.
In that case, you dispose the mask whenever you need to, but wipe off the permanent mask with peroxide wipes or whatever.
The problem with the first mask is that the outside of the filter cartridges is probably getting contaminated over time, and you don’t want that touching anything. The advantage is that one filter cartridge will last for a long time, and it won’t get soaked with moisture from the user’s breath.
This seems not so hard. What am I missing?
My guess is that medicine has a simple heuristic that you shouldn’t try to sanitize things that aren’t metal, especially if they are made of multiple materials. If you can make cheap disposable versions, just do it. But maybe that heuristic failed here.
How popular are disposable masks in industrial settings? I’d think that industrial workers trying to avoid dust or noxious fumes would have immediate feedback on fit and would learn to use them correctly. But if they use them everyday, they’d probably want the non-disposable version, anyhow.
Experience working as a maintenance technician for communal TV systems (which frequently brought me into contact with members of other trades on building sites) leads me to believe that most people in that sort of line of work will use as little PPE as they can possibly get away with, keeping it on hand to be hastily donned when the site supervisor comes round. Dust is generally preferred to masks or goggles.
Brazilian here: I went to an upper-middle class supermarket yesterday wearing a surgical mask. About ten percent of customers were wearing one as well, or something better. I don’t think I had ever seen Brazilians wearing surgical masks outside a hospital or other healthcare settings, and even then, mostly in ORs.
Not a single member of the staff was wearing one, however. And these are the people who are gonna talk to their well-traveled customers, get sick, show up for work feeling a little tired, and infect a whole bunch of other customers in their 50s and 60s, who in turn are shopping for their parents in their 70s and 80s.
When I went to the store on Monday, I was one of two people in the store wearing a mask. I think the other was an elderly Chinese lady.
Scott, I’d like to see your take on the protective effects of gloves.
As far as I can tell, wearing gloves is the same as getting one free handwashing — and the guidelines say to wash your hands after taking off the gloves anyway.
Gloves would protect against things entering your skin through cuts on the hand, which is a problem for some use cases but not for coronavirus.
This is unrelated to masks, however;
“Remember, there are dozens of studies supposedly showing homeopathy works”
Maybe there’s a reason for that?
There are two evidence-backed assumptions which, together, can explain the observed effects.
1. Diluting down a chemical using a single set of glassware will result in a small quantity of the material remaining, even with enough dilutions to theoretically remove all material.
2. Endocrine disruptors can exhibit a non-monotonic dose response curve. (I use rather unusual, technical language here because it returns better results from search engines.) In other words, human beings may be adapted to there being low levels of endocrine disruptors in their food. Plants commonly use such techniques in defense from various predators. Our bodies have adapted accordingly. So a tiny quantity of endocrine disruptor like, say, bisphenol-A is recognized as a signal. But a large quantity of bisphenol-A is recognized as noise and a problem and our body shuts the related system down.
Simply ignoring results when they don’t match our mental model can cause its own set of problems.
I’m wondering if more analysis is warranted? The evidence supporting wearing of masks seems compelling.
https://twitter.com/jeremyphoward/status/1242894386469486592
This for example tripped my spidey senses:
“They’re not airtight, so they offer no protection against airborne disease or the airborne component of aerosol diseases.”
I could see “minimal” or “limited”. But, none?
There are *some RCTs on surgical mask v N95 respirator efficacy in healthcare settings, though showing mixed results. (A friend asked me to take a peek at this recently out of curiousity, so I thought I’d mention 3 that I found here.)
C.R. MacIntyre, Q. Wang, B. Rahman, H. Seale, I. Ridda, Z. Gao, et al.
Efficacy of face masks and respirators in preventing upper respiratory tract bacterial colonization and co-infection in hospital healthcare workers
Prev Med, 62 (2014), pp. 1-7
MacIntyre, C. R., Wang, Q., Seale, H., Yang, P., Shi, W., Gao, Z., . . . Dwyer, D. E. (2013). A randomized clinical trial of three options for N95 respirators and medical masks in health workers. American Journal of Respiratory and Critical Care Medicine, 187(9), 960-6.
Loeb M, Dafoe N, Mahony J, John M, Sarabia A, Glavin V, Webby R, Smieja M, Earn DJD, Chong S, et al. Surgical mask vs N95 respirator for preventing influenza among health care workers: a randomized trial. JAMA 2009;302:1865-1871
Note – these studies look at influenza. Influenza virions are comparable enough to SARS-CoV-2 in size and make-up for the results to generalize. I think this because particle size differences around the ~50-200 microns range cause only small filter pentration differences for N95 respirators in a lab (see Bałazy, M. Toivola, A. Adhikari, S.K. Sivasubramani, T. Reponen, S.A. Grinshpun. Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks? Am. J. Infect. Control, 34 (2) (2006), pp. 51-57). Smaller particles probably travel more in the air though? I haven’t looked that up.
Btw, the author said “[o]verall I think modest reductions in particle number are still pretty good, but I don’t have a study that proves it” – I think an good RCT showing reduced infection rates due to mask use is good proof.
So the WHO has weighed in again, saying not to wear a mask, because of a false feeling of protection and can be a source of infection
https://twitter.com/WHOWPRO/status/1243171683067777024
Saw this the other night. This is put out by Fast.ai. Jeremy Howard is a data scientist and ethicist, co-founder of fast.ai (www.fast.ai.com) He includes studies comparing fabrics for “homemade” masks. Reports that in Czechoslovakia the whole population is encourage to wear masks when out. One of his commenters is a Czech who said it took 2 days to get over the social discomfort of wearing masks. I don’t know that the current numbers bear up to what he reports. (Poland reports very low numbers of cases.) Interesting read. #masks4all
https://youtu.be/BoDwXwZXsDI
Great analysis. Last days we have been researching the topic from another perspective, and I think the conclusions regarding the current situation are clear like water:
1. There are many asimptomatic patients of Covid-19.
2. Face masks (even surgical and homemade) may avoid that they spread the disease.
3. In many regions the supplies of surgical masks and respirators are wearing out, so they must be reserved for health professionals, care givers and alike.
4. People need to produce their own masks.
And here is where some info regarding basics, patterns, materials, etc. may come handy:
https://handgedacht.wordpress.com/2020/03/26/self-organization-of-personal-protection-and-that-of-the-population-diy-masks/
Take care!
Masks don’t cover the eyes. As mucus membranes, aren’t they vulnerable exposure points?
Interesting interview with George Gao, the head of the Chinese Center for Disease Control and Prevention: https://www.sciencemag.org/news/2020/03/not-wearing-masks-protect-against-coronavirus-big-mistake-top-chinese-scientist-says
The question and answer most relevant to this post:
Q [Cohen]: What mistakes are other countries making?
A [Gao]: The big mistake in the U.S. and Europe, in my opinion, is that people aren’t wearing masks. This virus is transmitted by droplets and close contact. Droplets play a very important role—you’ve got to wear a mask, because when you speak, there are always droplets coming out of your mouth. Many people have asymptomatic or presymptomatic infections. If they are wearing face masks, it can prevent droplets that carry the virus from escaping and infecting others.
Someone on the subreddit suggested masks made of cotton, dipped in brine and dried, were effective. Anyone heard more about this one?
Not tested, mere conjecture: Droplets = virus + water. Add soap and the virus is kaput. But brine does not make the pores of the mask smaller. So you can expect a lower number of virus particles to be still infectious after their carrier droplet has dried and they dust off again, but any household mask would be still be far from effective against inhaled aerosol. Brine is just an improvement that breaks a fraction of the virus load.
I think you mean ‘salt’.
And yeah, the idea is to improve effectiveness against droplet spread, not dry aerosol spread.
I really meant soap.
ETA: Washing powder brine might even be better, with its low-temperature protein cracking enzymes. But I’d worry about inhaling its dust.
The disagreement is not just whether someone gets infected but also on the recommendations derived from those facts. What I think really annoys people is the claim that general population should not buy and thus not wear masks at all.
https://twitter.com/Surgeon_General/status/1233725785283932160
If the messaging were that people should wear masks if they have them, perhaps even improvise some, but avoid buying them them because it’s a sad reality that there’s a shortage and it’s even more important for health professionals to have them that be far less contentious.
Also on stuff like “will people wearing the masks risk compensate in ways that put them more in danger” and “will most people screw up using the masks badly enough to lose the not-very-large benefit they provide?”
Is there an argument that your mask’s prevention of you touching your nose and mouth with dirty fingers provides much (or even all) of the benefit of wearing a mask — and that this might be a very big benefit indeed?
I made a very effective mask from a Melitta coffee filter: how-to-video.
Really enjoyed the article. A recent NY Times article covered this topic and linked an interesting study, not sure if you reviewed it as well:
https://www.nytimes.com/2020/03/17/opinion/coronavirus-face-masks.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2190272/
There is not room for hope when it comes to research. This is an absolutely absurd assumption to make, only made more palatable because the CDC made it first. Every study we have that shows that N95s help with the flu also show that surgical masks help. Every study we have that shows that surgical masks dont help also shows that N95s dont help either.
Swapping from science to hope halfway through a post is incredibly misleading and should be avoided at all costs.